AGEP Medication Risk Checker
Check Your Medication Risk
This tool helps you determine if a medication might cause AGEP (Acute Generalized Exanthematous Pustulosis), a rare but serious skin reaction triggered by medications. Remember: If you experience symptoms, stop the medication immediately and consult a healthcare provider.
What Is AGEP?
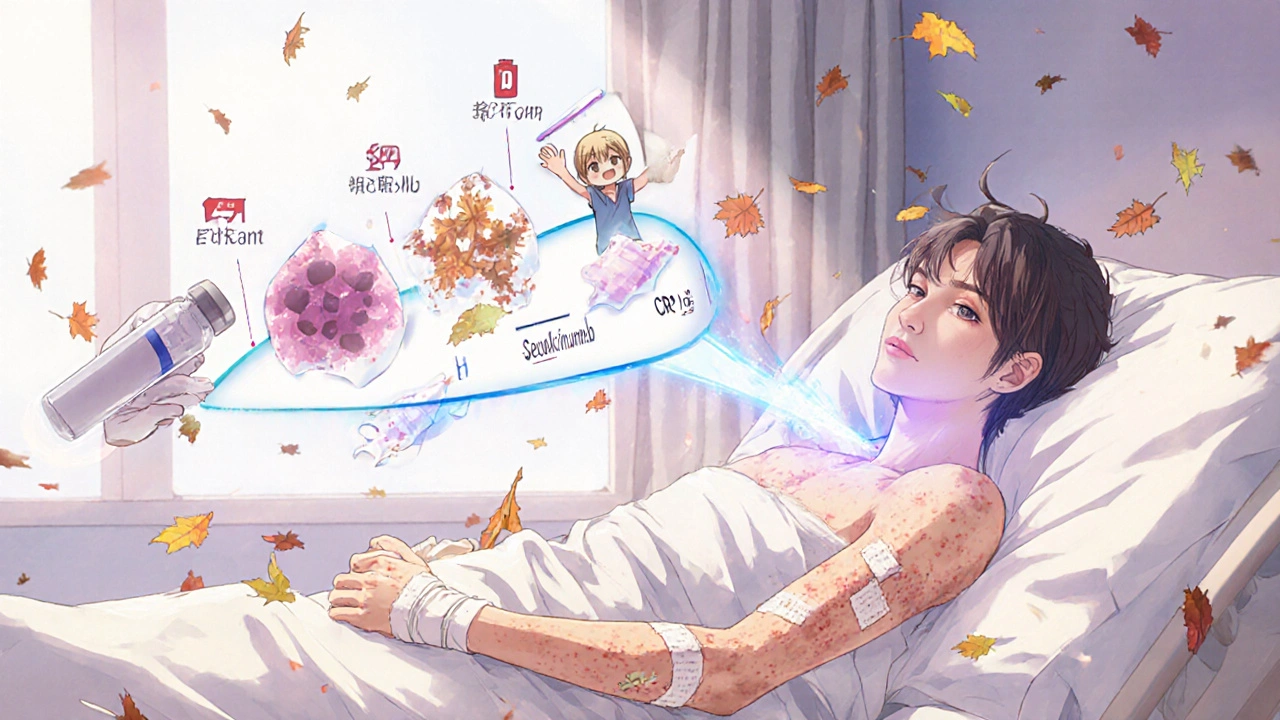
Acute Generalized Exanthematous Pustulosis (AGEP) is a rare but serious skin reaction triggered by medications, marked by the sudden appearance of hundreds of small, sterile pustules on red, inflamed skin. It doesn’t come from infection - the pus is made of white blood cells, not bacteria. Unlike acne or folliculitis, these pustules aren’t tied to hair follicles. They usually start in skin folds like the armpits, groin, or under the breasts, then spread quickly across the body within 24 to 48 hours.
AGEP was first clearly described in 1980, and since then, it’s been recognized as a distinct condition by the World Health Organization. It affects men and women equally, and while it’s most common in adults, it can happen at any age. The good news? Most people recover fully. The bad news? It can look terrifying - and it’s often mistaken for something worse.
How Fast Does It Show Up?
One of the clearest signs of AGEP is how fast it comes on. Most people notice the rash 1 to 5 days after taking a new medication, with the median being just 2 days. Some drugs, like amoxicillin-clavulanate, can trigger it even up to 14 days later - which makes it easy to miss the connection.
Imagine this: You take an antibiotic for a sinus infection. Three days later, you wake up with your skin burning, covered in tiny white dots that look like pimples but don’t pop. You have a low fever. Your skin feels tight. You go to your GP, who thinks it’s an allergic reaction or heat rash. But it’s not. It’s AGEP. And if you keep taking the drug, it gets worse.
What Causes AGEP?
More than 90% of AGEP cases are caused by drugs. The top offenders? Antibiotics - especially penicillins like amoxicillin and macrolides like erythromycin. Together, they cause over half of all cases. Antifungal meds like fluconazole come next, followed by calcium channel blockers used for high blood pressure.
Even more surprising? Some people develop AGEP from steroids - like prednisolone. Yes, the very drug meant to calm inflammation can trigger it. But here’s the twist: one patient in a 2023 study had AGEP from prednisolone, yet responded perfectly to methylprednisolone. That means not all steroids are the same, and switching types can sometimes work.
It’s not just about the drug - your genes matter too. A 2022 study found that people with the HLA-B*59:01 gene variant, common in Asian populations, are nearly 9 times more likely to develop AGEP after certain medications. This could one day lead to blood tests before prescribing high-risk drugs.
How Is It Different From Psoriasis?
Doctors often confuse AGEP with generalized pustular psoriasis - and that’s dangerous. The two look almost identical under the microscope. But they’re totally different in how they behave.
- AGEP: Comes on fast after a drug, clears in 10-14 days after stopping the trigger, rarely recurs.
- Pustular psoriasis: Often has a personal or family history of psoriasis, flares without drugs, lasts longer, and can be life-threatening.
AGEP usually spares the palms and soles - but psoriasis loves them. AGEP doesn’t have the target-shaped lesions you see in other rashes. And crucially, AGEP has a death rate of only 2-4%. Pustular psoriasis? Up to 25%.

What Do Labs Show?
There’s no single test for AGEP. Diagnosis is based on appearance, timing, and ruling out other causes. But blood tests help confirm it’s not infection or something else.
- White blood cell count is high - mostly neutrophils (often over 75% of total).
- C-reactive protein (CRP) is elevated, showing inflammation.
- Liver and kidney function are usually normal - unlike in other severe skin reactions like Stevens-Johnson Syndrome.
A skin biopsy can help, showing pustules just under the skin’s top layer, filled with neutrophils and sometimes eosinophils. But even that can look like psoriasis. So timing and drug history are just as important as the biopsy.
How Is AGEP Treated?
The single most important step? Stop the drug immediately. That’s it. In over 90% of cases, the rash starts fading within 2-3 days after stopping the trigger.
Supportive care is standard: cool compresses, moisturizers, antihistamines for itching, and keeping the skin clean. Hospital admission is recommended if you have a fever over 38.5°C, more than 20% of your skin covered, or signs of dehydration or organ stress.
Now the big debate: Do you use steroids?
Some experts say no. Dermatology Advisor, citing experience with 15 cases, says systemic steroids aren’t needed because AGEP clears on its own. Others - including a 2023 European panel - say yes, especially if the rash is widespread. Their data showed patients on oral prednisone (0.5-1 mg/kg/day) healed in 7 days, compared to 10-14 days without.
There’s no one-size-fits-all answer. If you’re otherwise healthy and the rash is mild, skip steroids. If you’re hospitalized, have a high fever, or the rash is spreading fast, steroids might help you get out of the hospital faster - by about 3 days on average.
What If Steroids Don’t Work?
For the rare cases that don’t improve, or if steroids aren’t safe (say, you have diabetes or high blood pressure), there are alternatives.
- Cyclosporine: An immune suppressant. Used at 3-5 mg/kg/day, it works as well as steroids but with fewer metabolic side effects.
- Secukinumab: A biologic drug that blocks IL-17, a key inflammation driver. In one case, a patient with AGEP from a blood pressure drug got completely better in 72 hours after one shot. Another study showed 92% of patients improved with no serious side effects.
These aren’t first-line - but they’re powerful tools for tough cases. Clinical trials for secukinumab and other IL-17 inhibitors are already underway, and early results look promising.
What Happens After the Rash Clears?
After 7-10 days, the pustules dry up and the skin starts peeling - like a bad sunburn. This is normal. But many patients don’t know this is part of healing. They panic, thinking it’s getting worse.
Use gentle, fragrance-free moisturizers. Avoid sun exposure - damaged skin burns easily. One 2022 study found that patients given written instructions on aftercare had a 78% compliance rate. Those who only got verbal advice? Only 42% followed through.
Keep a list of all medications you took before the rash. Avoid them forever. Even if you think you’re fine, re-exposure can cause AGEP again - and next time, it could be worse.
Why Is This Underdiagnosed?
Studies show up to 40% of AGEP cases are misdiagnosed in community clinics. Why? Most doctors see one or zero cases in their career. They don’t recognize the pattern. They think it’s a viral rash, fungal infection, or allergic reaction.
Specialist dermatology centers get it right 90% of the time. The new AGEP Probability Score (APS), developed by the EuroSCAR group, helps - it uses 8 clinical features to give a score. With 94% sensitivity, it’s becoming a standard tool in teaching hospitals.
But outside those centers? Many hospitals don’t have AGEP protocols. No checklists. No clear guidance. That’s why delays happen - and delays mean longer hospital stays (5.7 to 9.3 days on average).
What’s Changing in AGEP Care?
Big changes are coming. The European Medicines Agency now requires drug makers to monitor for AGEP in clinical trials - especially for antibiotics and heart meds. Amoxicillin-clavulanate’s label was updated in 2021 to include AGEP as a known risk.
Research is exploding. In 2018, there were 15 papers on AGEP. In 2022, there were 42. The International Registry (RegiSCAR) has tracked over 300 cases since 2020, with 5-year follow-ups planned. That’s how we’ll learn long-term outcomes.
And the future? Genetic screening. Personalized drug choices. Biologics as first-line for severe cases. We’re moving from reactive care to predictive prevention.
What Should You Do If You Suspect AGEP?
- Stop the new medication immediately - don’t wait for a doctor’s note.
- Go to urgent care or the ER if you have fever, widespread rash, or feel unwell.
- Bring a list of all medications you took in the last 2 weeks - even supplements.
- Don’t pop pustules. Don’t use strong soaps or scrubs.
- Ask for a dermatology consult if you’re in hospital.
Most people recover fully. But missing the diagnosis - or delaying treatment - can lead to longer hospital stays, unnecessary antibiotics, or even misdiagnosis as psoriasis, which changes your lifelong care plan.
Is AGEP contagious?
No, AGEP is not contagious. The pustules are sterile - they contain your body’s own white blood cells, not bacteria or viruses. You cannot spread it to others through touch, air, or bodily fluids.
Can AGEP come back after it clears?
It’s rare, but possible - only if you take the same drug again. Once you’ve had AGEP from a specific medication, you must avoid it for life. Re-exposure can cause a more severe reaction, sometimes fatal.
How long does AGEP last?
The rash typically peaks within 2-3 days and starts fading after stopping the drug. Full recovery - including peeling and skin healing - takes 10 to 14 days on average. Hospital stays average 5-9 days, depending on severity.
Are over-the-counter creams safe for AGEP?
Avoid steroid creams unless prescribed. OTC hydrocortisone is too weak to help and may delay proper diagnosis. Use fragrance-free moisturizers and cool compresses instead. If itching is bad, oral antihistamines like cetirizine are safe and helpful.
Can children get AGEP?
Yes, though it’s rare. Children account for less than 5% of reported cases. The triggers are similar - antibiotics are the most common. Pediatric cases require careful monitoring, as their bodies react differently to medications and fluids.
What drugs are most likely to cause AGEP?
Antibiotics cause over 50% of cases, especially amoxicillin-clavulanate, erythromycin, and sulfonamides. Antifungals like fluconazole, calcium channel blockers like diltiazem, and even some NSAIDs can trigger it. Always consider any new drug taken in the last 2 weeks.
Is AGEP life-threatening?
It can be, but it’s rare. The death rate is 2-4%, mostly in elderly patients or those with other illnesses. The main risks are infection from broken skin, fluid loss, or organ stress. Prompt diagnosis and stopping the drug reduce risk dramatically.
Should I get genetic testing for AGEP risk?
Not yet - it’s still in research. The HLA-B*59:01 gene is linked to higher risk in Asian populations, but testing isn’t routine. If you’ve had AGEP before, avoid the triggering drug. Genetic screening may become standard in the next 5-10 years.





Archana Jha
soooo... you're telling me big pharma is secretly using AGEP as a way to test our immune systems? like... they give us amoxicillin and wait to see who breaks out in pustules? i mean, why else would they push it so hard? plus, did you know the WHO is actually just a front for the Illuminati? they love pustules. 🤫🩸
Aki Jones
Okay, but let’s be precise: AGEP is not a ‘rash’-it’s a dysregulated neutrophilic cytokine storm triggered by haptenization of drug metabolites via HLA class I presentation. The fact that 90% of cases are drug-induced doesn’t mean it’s ‘allergic’-it’s an innate immune misfire. And yes, the HLA-B*59:01 association is statistically significant (p<0.001), but no one in primary care knows this. Why? Because the FDA doesn’t mandate pharmacogenomic screening. And that’s a systemic failure.
Jefriady Dahri
this is actually super important info 😊 i had a cousin who got this after taking amoxicillin and everyone thought it was just a weird allergy. she was in the hospital for 8 days and no one knew what was going on. if more people knew this, maybe they wouldn’t have given her steroids right away. thank you for explaining it so clearly! 🙏
Andrew McAfee
so basically if you take antibiotics in India you might get pustules because of your genes and then you get blamed for not knowing your body but in america we just call it a rash and move on
Andrew Camacho
LET ME TELL YOU SOMETHING. THE PHARMA COMPANIES KNOW EXACTLY WHAT THEY’RE DOING. THEY’RE NOT JUST SELLING DRUGS - THEY’RE TESTING HUMAN SUSCEPTIBILITY. DID YOU KNOW THAT FLUCONAZOLE WAS MARKETED FOR YEARS BEFORE ANYONE REALIZED IT COULD TRIGGER AGEP? THAT’S NOT AN ACCIDENT. THAT’S A CALCULATED RISK. AND NOW THEY WANT YOU TO TAKE ‘SECUKINUMAB’ LIKE IT’S A LIFESTYLE PRODUCT? NOPE. I’M NOT BUYING IT. 🤬
Arup Kuri
people these days take meds like candy. you think its just a pill so what? you dont even know what you put in your body. i told my niece dont take that amoxicillin stuff and she laughed. now she has pustules all over her. this is why india is falling behind. no discipline. no responsibility. just pills pills pills
Elise Lakey
I’m curious-how often do patients actually get follow-up genetic testing after an AGEP episode? I’ve never heard of anyone being offered it, even in big hospitals. Is it just not available, or do doctors not think it’s worth it? I’d love to know if there’s any data on long-term tracking.
Erika Hunt
I think what’s really interesting here is how the medical community has this huge gap between what’s known in dermatology research centers and what’s happening in rural clinics or even small-town ERs. Like, the AGEP Probability Score sounds amazing, but if your doctor has never even heard of AGEP, they’re just going to slap on some hydrocortisone and send you home. And then you come back two weeks later with peeling skin and they’re like, ‘Oh, that’s normal?’ No, it’s not. It’s a systemic failure in education, communication, and access to specialist knowledge.
Lisa Odence
The data presented here is scientifically robust, yet the dissemination mechanisms remain profoundly inadequate. The integration of pharmacogenomic screening into primary care workflows is not merely a clinical recommendation-it is an ethical imperative. The fact that HLA-B*59:01 testing is not standard-of-care for patients of Asian descent prior to antibiotic administration constitutes a violation of the principle of non-maleficence. Furthermore, the normalization of ‘watchful waiting’ in the face of a potentially fatal reaction is a failure of medical governance.
Patricia McElhinney
This article is dangerously misleading. You say AGEP is 'rare' - but you ignore the fact that most cases go unreported because doctors misdiagnose it as psoriasis or fungal infection. And now you're recommending steroids? Are you kidding me? Steroids suppress immunity - and what if you have an undiagnosed TB? Or HIV? You're putting lives at risk with this 'one-size-fits-all' advice. This is why people die. Because doctors trust guidelines instead of thinking. 😒
Dolapo Eniola
in nigeria we dont even have dermatologists in half the hospitals but you people in usa talk about secukinumab like its a new iphone. we dont even have amoxicillin in some villages. you think your gene testing matters when your kid is crying because the fever wont go down? stop talking about science and fix the basics first. 🇳🇬✊
Agastya Shukla
The HLA-B*59:01 association is fascinating from a pharmacogenomics standpoint - especially since it’s more prevalent in South Asian populations. But I wonder if environmental co-factors like gut microbiome composition or concurrent infections modulate the risk. There’s a 2023 preprint from Mumbai suggesting that prior exposure to helminths might downregulate the neutrophilic response. Could that explain regional variation in incidence?
Pallab Dasgupta
bro i had this once after taking that amoxicillin for my tooth infection. i thought i was gonna die. skin on fire. felt like i was covered in pop rocks. went to the doc and they said 'it's just a rash'. i said 'no bro this is AGEP' and they looked at me like i was crazy. then i showed them the article on my phone and they were like 'ohhhhh'. i was out in 7 days. but man - if i hadn't read this stuff? i'd still be in the hospital crying. so yeah. this post saved my life. 🙌🔥
Rachel Villegas
I’m so glad someone finally explained the difference between AGEP and pustular psoriasis. I’ve been terrified for months thinking I might have psoriasis because of the pustules. Now I know it was just the antibiotic I took. Relief.
Leisha Haynes
so you're telling me the cure for AGEP is to stop the drug... and also maybe take a billion dollar biologic that no one can afford? lol. brilliant. next you'll tell me the solution to heart disease is to stop eating and then get a $200k stent. classic medicine. 🙃