DOAC Dosing Calculator for Kidney Impairment
Calculate Your DOAC Dose
Select your DOAC medication and input your kidney function parameters to determine the correct dose. Based on FDA guidelines and clinical studies.
Results
Why DOACs Are Tricky When Your Kidneys Aren’t Working Right
Direct Oral Anticoagulants, or DOACs, are the go-to blood thinners for people with atrial fibrillation. They’re easier than warfarin-no weekly blood tests, fewer food interactions, and more predictable results. But here’s the catch: if your kidneys aren’t functioning well, these same drugs can turn dangerous. About one in three patients with atrial fibrillation also have chronic kidney disease. That’s not rare. It’s common. And if you’re taking a DOAC like apixaban, rivaroxaban, or dabigatran without adjusting the dose for poor kidney function, you’re playing Russian roulette with bleeding or clots.
How DOACs Leave Your Body (And Why It Matters)
Unlike warfarin, which is broken down by the liver, most DOACs are cleared by the kidneys. That means if your kidneys are weak, the drug builds up in your system. Too much? Risk of major bleeding-brain bleeds, stomach bleeds, even fatal internal bleeding. Too little? Clots form. Strokes happen. That’s why dosing isn’t one-size-fits-all. It’s not about how you feel. It’s about how well your kidneys filter blood.
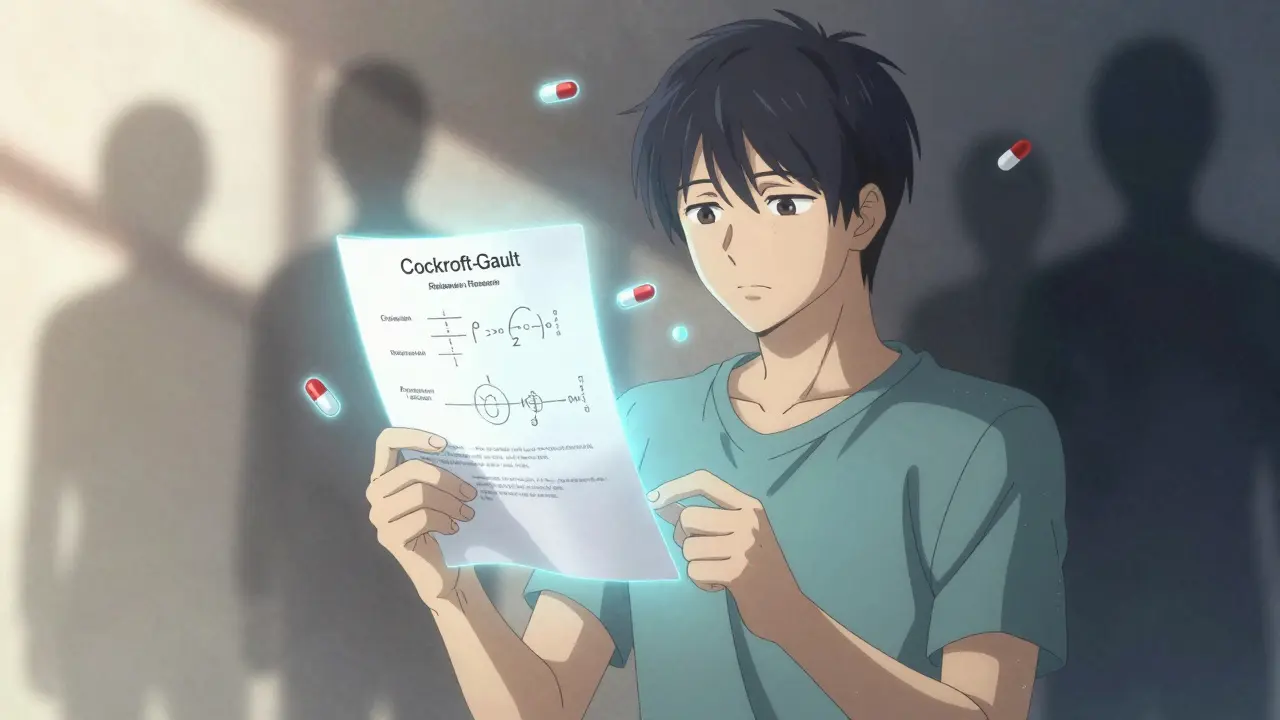
The gold standard for measuring this isn’t the eGFR number your doctor sees on your lab report. It’s the Cockcroft-Gault formula. That’s right-older, clunkier, but still the only one the FDA and major guidelines accept for DOAC dosing. Why? Because eGFR doesn’t account for muscle mass or body weight the same way. In elderly patients, especially those thin or frail, eGFR can overestimate kidney function by 20% or more. That’s enough to give someone the wrong dose-and put them at risk.
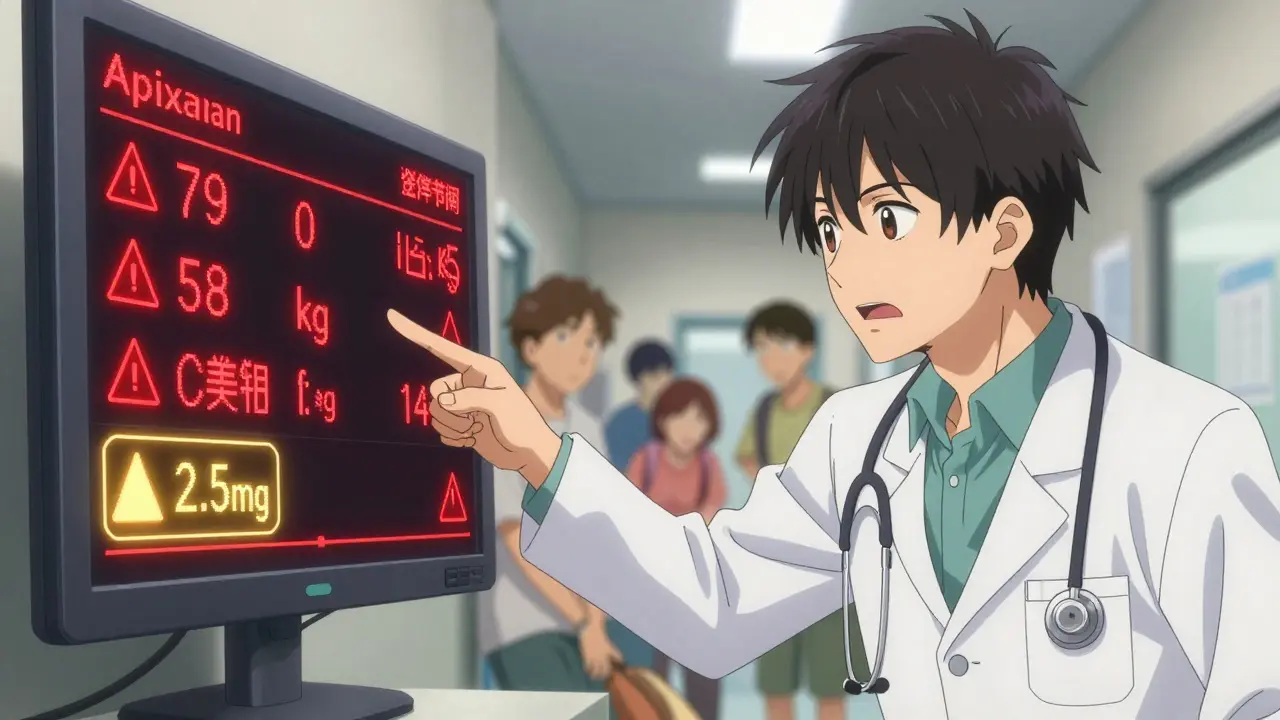
Apixaban: The Safest Bet for Kidney Problems
Among all DOACs, apixaban (Eliquis) stands out. It’s the only one with a clear safety profile even in end-stage kidney disease. Studies show it causes less bleeding than warfarin in patients on dialysis. The FDA allows its use in CrCl as low as 15 mL/min, and even below that, many nephrologists use it off-label because there’s no better option.
But here’s the fine print: you can’t just give the standard 5 mg twice daily. You need to cut it to 2.5 mg twice daily if you meet any two of these three criteria:
- Age 80 or older
- Body weight 60 kg or less (about 132 lbs)
- Serum creatinine 133 μmol/L or higher (1.5 mg/dL)
That’s not optional. That’s mandatory. A 2022 JAMA Internal Medicine study found that nearly 4 in 10 DOAC prescriptions in kidney patients were wrong-and apixaban was the most commonly misprescribed. Why? Doctors forget the rules. Or they assume eGFR is enough. Or they don’t check weight or age.
Rivaroxaban and Dabigatran: Use with Extreme Caution
Rivaroxaban (Xarelto) should not be used if your CrCl is below 15 mL/min. Period. No exceptions. Even at CrCl 15-30 mL/min, you need to drop the dose from 20 mg daily to 15 mg daily. But many patients are still getting the full dose. That’s why bleeding rates spike in this group.
Dabigatran (Pradaxa) is even more kidney-dependent. If your CrCl is between 15 and 30 mL/min, you must reduce it to 75 mg twice daily. Below 15? Don’t use it. It’s contraindicated. Yet, in community clinics, I’ve seen patients on dialysis still taking dabigatran-because the pharmacist didn’t flag it, or the chart didn’t show the CrCl clearly.
Edoxaban: Narrow Window, Big Risk
Edoxaban (Savaysa) is only approved for CrCl above 15 mL/min. If your CrCl is between 15 and 50 mL/min, you cut the dose from 60 mg daily to 30 mg. Below 15? Avoid it. The ENGAGE AF-TIMI 48 trial showed edoxaban loses effectiveness in patients with poor kidney function. That means you’re getting the bleeding risk without the protection.
Warfarin Still Has a Role-But Only in Severe Cases
Many assume warfarin is outdated. But in end-stage kidney disease (CrCl <15 mL/min), it’s still a tool. Not because it’s better-but because the alternatives are risky or unproven. Studies show warfarin causes more brain bleeds and vascular calcification in dialysis patients. But it’s predictable. You can monitor it. And if your kidney function is dropping fast, warfarin gives you more control.
The American Heart Association still lists warfarin as an option for ESRD patients. But here’s the truth: most cardiologists avoid it. It’s messy. Diet changes. Drug interactions. Frequent INR checks. But if you’re on dialysis and your CrCl is below 15, and you can’t get apixaban safely adjusted-warfarin might be the least bad choice.
What You Need to Do Right Now
Stop guessing. Start calculating.
- Get your creatinine level from your last blood test.
- Know your age, sex, and weight in kilograms.
- Use the Cockcroft-Gault formula: (140 - age) × weight (kg) × (0.85 if female) / (72 × serum creatinine)
- Don’t trust eGFR. Use this number.
- Match your CrCl to the DOAC dosing chart below.
Quick Dosing Guide for DOACs in Renal Impairment
| DOAC | Standard Dose | CrCl 15-29 mL/min | CrCl <15 mL/min or on dialysis |
|---|---|---|---|
| Apixaban | 5 mg twice daily | 2.5 mg twice daily (if ≥2 criteria met) | 2.5 mg twice daily (safe; no contraindication) |
| Rivaroxaban | 20 mg once daily | 15 mg once daily | Contraindicated |
| Dabigatran | 150 mg twice daily | 75 mg twice daily | Contraindicated |
| Edoxaban | 60 mg once daily | 30 mg once daily | Contraindicated |
Remember: for apixaban, the 2.5 mg dose isn’t just for CrCl 15-29. It’s also for anyone over 80, under 60 kg, or with creatinine ≥1.5 mg/dL-even if their CrCl is normal. That’s the ABC rule: Age, Body weight, Creatinine. If two apply, cut the dose.
What Happens When You Get It Wrong
There’s a case from a Sydney hospital last year. A 79-year-old woman, weight 58 kg, creatinine 145 μmol/L, CrCl 22 mL/min. She was on apixaban 5 mg twice daily. She had a massive GI bleed. Turned out, she met all three ABC criteria. Should’ve been on 2.5 mg. She survived-but barely. Her family had to sell their house to pay for the ICU stay.
Another patient, 82, on rivaroxaban 20 mg daily, CrCl 12 mL/min. No adjustment. He had a stroke. The blood thinner didn’t work because his kidneys weren’t clearing it properly-it was sitting in his blood, not helping. The dose was too high, but the effect was too low. That’s the paradox of renal impairment.
What’s Changing in 2025-2026
Two big trials are wrapping up. The RENAL-AF trial is comparing apixaban to warfarin in patients with CrCl under 30 mL/min. Results expected in 2025. The AXIOS trial, though stopped early, will release data on apixaban in dialysis patients in late 2024. Early signs? Apixaban may be the only DOAC that’s truly viable for advanced kidney disease.
By 2026, guidelines will likely tighten. We’ll see more clear rules for dialysis patients. But for now? The safest move is this: if you have kidney disease and need a blood thinner, start with apixaban. Cut the dose if you’re old, small, or have high creatinine. Avoid rivaroxaban, dabigatran, and edoxaban if your CrCl is below 30. And always, always check your CrCl with Cockcroft-Gault-not eGFR.
What Your Pharmacist Should Be Checking
Pharmacists are your last line of defense. If your doctor prescribes a DOAC and you have kidney disease, ask: "Did you use Cockcroft-Gault? Did you check my age, weight, and creatinine?" If they say "I used the eGFR," walk out and get a second opinion. A 2022 study found that nearly 3 out of 10 elderly patients had their CrCl miscalculated because no one adjusted for low muscle mass. That’s not negligence. It’s ignorance. And it’s deadly.
Virtual anticoagulation clinics are helping. They track your labs, flag changes, and auto-adjust doses. If your clinic offers one-use it. If not, ask your doctor to refer you. It’s not a luxury. It’s a safety net.
Final Thought: Don’t Assume Your Doctor Knows
Even experienced cardiologists miss this. A 2023 survey of 400 U.S. doctors found that 41% couldn’t correctly identify the CrCl cutoff for apixaban dose reduction. That’s not a small error. That’s a systemic problem.
You’re not just a patient. You’re your own advocate. Know your numbers. Know your drugs. Ask the questions. Because when your kidneys fail, your blood thinner can’t afford to be wrong.
Can I take a DOAC if I’m on dialysis?
Yes-but only apixaban. Rivaroxaban, dabigatran, and edoxaban are contraindicated. Apixaban is the only DOAC with data showing it’s safe at a reduced dose (2.5 mg twice daily) even for patients on hemodialysis. Warfarin is still an option, but apixaban causes fewer bleeds and doesn’t require frequent blood tests.
Why can’t I just use eGFR instead of Cockcroft-Gault?
eGFR estimates how well your kidneys filter waste, but it doesn’t account for body weight or muscle mass. In older, thin, or frail patients, eGFR often overestimates kidney function. The FDA and all major guidelines require Cockcroft-Gault for DOAC dosing because it’s more accurate for predicting how the drug will clear from your body. Using eGFR could give you a dangerously high dose.
What if my creatinine is normal but I’m 80 and weigh 55 kg?
You still need to reduce your apixaban dose to 2.5 mg twice daily-even if your CrCl is above 30. The ABC rule (age ≥80, weight ≤60 kg, creatinine ≥1.5 mg/dL) applies. If you meet two of these, the dose must be cut. This is based on real-world data showing higher bleeding risk in these patients, even with normal kidney function.
Is warfarin safer than DOACs in advanced kidney disease?
Not necessarily. Warfarin increases the risk of brain bleeds and calcium buildup in blood vessels in dialysis patients. But because DOAC data is limited in this group, warfarin remains an option when DOACs can’t be safely used. Apixaban is now preferred over warfarin in most cases-even in ESRD-because it’s easier to manage and has better safety data.
How often should my kidney function be checked if I’m on a DOAC?
At least once a year. But if you’re over 75, have diabetes, or have known kidney disease, check every 3-6 months. Kidney function can decline quickly. A drop from CrCl 40 to 25 in six months changes your dose. Waiting a year could be dangerous.
Can I switch from warfarin to a DOAC if I have kidney disease?
Yes-if your CrCl is above 30 mL/min. Apixaban is the best choice. If your CrCl is below 30, you can still switch-but only to apixaban at the reduced dose. Never switch to rivaroxaban, dabigatran, or edoxaban if your kidneys are impaired. Always check your CrCl with Cockcroft-Gault before switching.




Kerry Howarth
Apixaban at 2.5 mg BID when you hit two of those three criteria isn't optional-it's life-saving. Saw a patient bleed out because someone skipped the weight check. Don't be that doctor.
Tiffany Channell
The fact that eGFR is still used instead of Cockcroft-Gault is criminal. Medical education is broken if you're teaching residents to trust automated eGFR without questioning it.
Joy F
We're treating kidneys like they're just a filter, but they're a symphony. When one instrument's out of tune-creatinine, age, weight, muscle mass-the whole piece collapses. And we're still playing the same score from 1987 while the world changed. Dabigatran in dialysis patients? That's not negligence. That's ritualistic disregard dressed as protocol.
Haley Parizo
This isn't about dosing. It's about power. Who gets to decide what 'safe' means? Pharma reps? Hospital algorithms? Or the actual human being with two kidneys that barely work? We've turned medicine into a spreadsheet and called it science.
Ian Detrick
Honestly, apixaban being the safest option makes sense. It's got that dual clearance-kidneys and liver. Less dependency means less chaos when things go south. Still, I wish more docs would actually run the Cockcroft-Gault instead of just eyeballing it.
Angela Fisher
I know someone who died from a brain bleed after being on Xarelto. The hospital didn't even check his CrCl. They said 'he looked fine.' Looked fine? He was 82, 55kg, and his creatinine was 2.1. They gave him 20mg. That wasn't an error. That was a death sentence wrapped in a prescription pad. And now they're still doing it. They're ALL still doing it.
Neela Sharma
In India we see this every day-old folks on DOACs because the family wanted something 'new' and 'easy.' No one checks weight. No one asks about diet. No one calculates. We give pills like candy. Then we wonder why the hospital fills up with bleeding patients. It's not medicine. It's superstition with a stethoscope.
Shruti Badhwar
The JAMA study cited is critical. Misprescribing rates above 40% for apixaban in CKD patients indicate systemic failure in clinical decision support. Electronic health records must be updated to trigger mandatory dose adjustments based on Cockcroft-Gault, weight, and age thresholds. This is not optional clinical judgment-it is a safety imperative.
Brittany Wallace
I just had my grandpa on apixaban 2.5mg after they realized he was 83, 58kg, and his creatinine was 1.6. He cried because he thought he was going to die from a stroke. Now he’s walking again. Thank you for writing this. Someone needed to say it out loud.
Michael Burgess
I'm a pharmacist. I've caught over 30 wrong DOAC doses in the last year. Half of them were apixaban. Doctors think 'lower dose' means 'half the pill' and don't realize it's a specific formulation. I've had to call 12 times just to get a 2.5mg script written correctly. We need better alerts. And maybe a badge for docs who know Cockcroft-Gault by heart.
Liam Tanner
Warfarin’s not dead. It’s just quiet. I had a dialysis patient on it for 7 years. Stable INR, no bleeds. He hated the blood tests but lived. Sometimes the old way is the right way when the new way has too many blind spots.
Palesa Makuru
You know what’s worse than wrong dosing? When the patient doesn’t even know they’re on a blood thinner. I had a lady who didn’t know she was on Pradaxa-her daughter filled the script and never told her. She fell, hit her head, and ended up in the ER with a subdural. No one asked about meds. No one checked. This isn’t medicine. It’s negligence theater.
Hank Pannell
The real tragedy isn't the dosing errors-it's that we treat kidney function like a static number. But it’s dynamic. A 70-year-old with sarcopenia? Their creatinine might be normal but their muscle mass is gone. Their true CrCl is half what the eGFR says. We need point-of-care tools that factor in body composition, not just serum creatinine. This is 2025. We should be doing better.
Lori Jackson
Let’s be honest-most of these guidelines exist because lawsuits happened. Not because doctors care. The FDA didn’t change rules because they love patients. They changed them because someone died, and the lawyer had the chart. Medicine is now liability-driven, not science-driven.
Wren Hamley
I used to think DOACs were magic. Then I saw a 79-year-old woman with CrCl 18 on rivaroxaban 20mg daily. She bled into her abdomen. She survived. But her husband asked me, 'Why didn't anyone just check?' That question haunts me. We’re not just prescribing drugs. We’re betting lives on a number we don’t even understand.