Injection Site Rotation Planner
Why This Matters
Lipodystrophy and bruising aren't just cosmetic issues—they affect insulin absorption and blood sugar control. Research shows that 78% of lipohypertrophy cases occur in the abdomen, and 90% of users experience bruising. Proper rotation prevents these complications.
According to the article, you should rotate at least 1 inch (2.54 cm) from your last injection site. This tool helps you track your sites and avoid overlapping areas.
How to Use This Tool
Click on the body areas below to mark your injection sites. The tool will calculate your spacing and alert you to potential issues. Remember: never inject within 1 inch of a previous site.
Important: For best results, rotate your injection sites weekly. Never inject within 1 inch (2.54 cm) of a previous injection site. If you inject in the same area repeatedly, you risk developing lipohypertrophy or bruising.
Current Rotation Status
Your current rotation pattern is acceptable.
Rotation Tips
When rotating injection sites:
- Always inject at least 1 inch (2.54 cm) away from previous sites
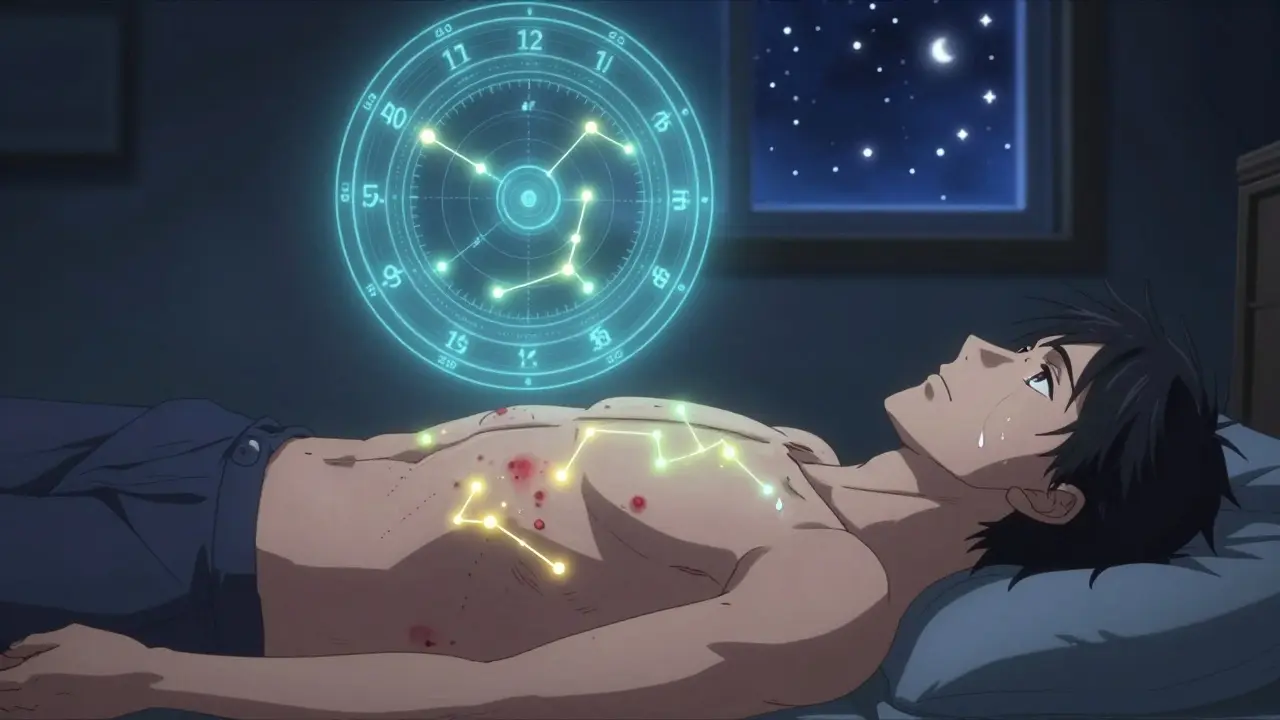
- Use a clock face method (12 o'clock, 3 o'clock, etc.) for precise rotation
- Check your sites for lumps or bruising before injecting
- Never reuse the same needle
- Don't press too hard when injecting
Every time you inject insulin, your body doesn’t just absorb the medicine-it also reacts to the needle, the pressure, and the repeated trauma in the same spot. For many people with diabetes, this leads to two silent but serious problems: lipodystrophy and bruising. These aren’t just skin deep. They can throw your blood sugar into chaos, make insulin less effective, and increase your risk of dangerous highs and lows. And yet, most doctors never check for them.
What Lipodystrophy Really Looks Like
Lipodystrophy isn’t one thing. It’s two opposite reactions happening in the same place: fat growing or fat disappearing. The most common form is lipohypertrophy-a soft, rubbery lump under the skin where you’ve injected insulin over and over. These lumps can be as big as a golf ball. They don’t hurt. They don’t turn red. That’s why people keep using them. Why? Because they feel numb. Less pain = better injection, right? Wrong. Insulin doesn’t absorb evenly from these lumps. It’s slow. Unpredictable. One day you get a low because it absorbed too fast. The next day, your blood sugar spikes because it barely moved. Studies show people with lipohypertrophy need 20-30% more insulin just to get the same effect. That’s not just wasteful-it’s dangerous. The other side is lipoatrophy. This is rare now, but it still happens. Instead of fat building up, it vanishes. You get a shallow dent in your skin, like a crater. It’s caused by an immune reaction to older insulin types, mostly animal-based or poorly purified human insulins. Most people today won’t see this unless they’ve been on insulin for decades with outdated products.Why You Keep Getting Bruises
Bruising isn’t rare. In fact, nearly 66% of insulin users report it. But it’s not always the needle’s fault. A 2023 study found that 901 out of 1,370 people had visible bruising after injections. The real culprit? Pressure. Most people press the pen too hard. They think pushing down makes the shot go in better. But that’s not how it works. The needle’s short-just 4 to 8 millimeters. If you press hard, you’re squeezing the skin and pinching blood vessels underneath. That’s what causes the bruise. It’s not hitting a vein-it’s crushing tissue. And here’s the kicker: repeated bruising can turn into lipohypertrophy. Gentile’s research calls bruising a “preliminary stage” of fat buildup. Each time you bruise the same spot, your body starts laying down scar tissue and fat to heal. It’s a slow creep. You don’t notice it until the lump is big enough to see.Where It Happens-and Why It Matters
Lipohypertrophy doesn’t show up randomly. 78% of cases are in the abdomen. Why? Because it’s easy to reach. You don’t need to twist. You don’t need to ask for help. But that’s also why it’s the most dangerous place to reuse. The thighs come second, at 22%. But people rarely rotate between them. They stick to the front of the thigh, then the inner thigh, then the same spot again. Same with the arms and buttocks. You think you’re rotating because you’re moving from “stomach” to “thigh.” But if you’re still hitting the same 2-inch circle, you’re not rotating at all. Your body doesn’t care about zones. It cares about exact spots. If you inject within 1 inch of the same point three times a week, you’re building a lump. The skin doesn’t heal fast enough. Fat cells swell. Collagen builds up. And insulin? It gets trapped.
The Real Cost: Blood Sugar Chaos
This isn’t just about ugly lumps. It’s about your A1c. One patient in a Diabetes Daily forum shared that after years of injecting in the same abdominal spot, her A1c jumped from 7.2% to 8.9%-without changing her diet, activity, or insulin dose. That’s a 23% increase in average blood sugar. That’s a higher risk of nerve damage, kidney stress, vision loss. And the hypoglycemia? It’s worse. People with lipohypertrophy have 3.2 times more unexplained lows. Why? Because insulin absorption is erratic. One injection might release all at once. The next might barely register. Your body can’t adapt. You end up guessing your doses. You start overcorrecting. You spiral. Even worse, you’re 2.7 times more likely to end up in diabetic ketoacidosis (DKA) because your body thinks it’s not getting enough insulin-when really, it’s just getting it too late.How to Fix It: The 4-Step Plan
You can stop this. But it takes more than willpower. It takes a system.- Inspect every injection site. Before you inject, feel the area with your fingers. Run them over your abdomen, thighs, arms. Look for lumps, ridges, or dents. If it feels different from the rest of your skin-softer, firmer, bumpy-don’t inject there. Mark it. Avoid it for at least 4 weeks.
- Rotate with precision. Don’t just move from stomach to thigh. Move at least 1 inch (2.54 cm) from your last injection point. Use a grid. Think of your abdomen as a clock. Monday: 12 o’clock. Tuesday: 3 o’clock. Wednesday: 6 o’clock. Thursday: 9 o’clock. Friday: back to 12, but 1 inch out. Repeat. Don’t reuse a spot for 4-8 weeks.
- Use a fresh needle every time. Reusing needles isn’t saving money-it’s making lumps. A blunt needle tears tissue. It causes more bruising. It increases infection risk. Even if the needle looks sharp, the coating wears off. Switch every single time. It’s cheaper than fixing your blood sugar.
- Don’t press hard. Let the pen do the work. Hold it perpendicular. Press gently until you hear the click. Hold for 10 seconds. Then lift straight up. No rubbing. No massaging. That’s what causes bruising.
Tools That Actually Help
You don’t have to remember this alone. There are tools built for this. Apps like InPen track your injection sites with GPS-like accuracy. You tap where you injected, and it shows you where you’ve been. It won’t let you pick a spot too soon. It’s rated 4.7 out of 5 by over 1,200 users. Many say it cut their unexplained lows by 80% in three months. Some insulin pumps now come with built-in site tracking. Medtronic’s MiniMed 780G logs injection locations and suggests new spots. It’s not perfect, but it’s a start. YouTube channels like “All About Diabetes” have short videos showing exactly how to feel for lumps and how to rotate properly. One viewer said after watching the rotation demo, her bruising dropped by 92%.Why Your Doctor Might Not Mention It
Here’s the uncomfortable truth: most doctors don’t check injection sites. A 2023 survey found 61% of patients said their provider never examined their injection areas-even after 5+ years of insulin use. Why? Because they’re not trained to. Medical schools rarely teach injection site assessment. Insurance doesn’t pay for it. Time is short. But that doesn’t mean you shouldn’t ask. Next time you’re in, say: “Can you check my injection sites? I’m worried about lumps or bruising.” Bring your log. Show them your app data. If they look confused, you’re not alone. But you’re also not wrong.What’s Next: The Future of Injection Safety
The field is changing. In 2023, Abbott announced a new biosensor in development that will monitor injection site health in real time-detecting early fat buildup before it becomes visible. It’s expected in 2025. AI tools like Glooko’s site-mapping system already cut lipodystrophy rates by 31% in a 6-month trial. These aren’t sci-fi. They’re here. But the biggest change won’t come from tech. It’ll come from awareness. When more people know that a lump isn’t harmless-that a bruise isn’t just bad luck-that a needle isn’t a one-time tool-then things will get better. You’re not just injecting insulin. You’re managing your body’s response. Every spot matters. Every needle counts. And your blood sugar is watching.Can lipodystrophy go away on its own?
Yes-but only if you stop injecting in that spot. Lipohypertrophy can shrink over time if you avoid the area for 3-6 months. Lipoatrophy is slower to recover and may leave a permanent dent. The key is consistency: once you stop injecting there, your body starts healing. But if you keep using it, the lump will grow larger and harder.
Is bruising dangerous?
Bruising itself isn’t dangerous, but it’s a warning sign. It means you’re pressing too hard or reusing the same spot too often. Left unchecked, it can lead to lipohypertrophy, which directly affects insulin absorption and causes dangerous blood sugar swings. It’s not the bruise you need to worry about-it’s what the bruise is telling you about your technique.
Can I still inject in areas with mild bruising?
No. Wait until the bruise is completely gone and the skin feels normal again. Injecting over a bruise increases the risk of deeper tissue damage and can trigger fat buildup. Use a different site, even if it’s inconvenient. Your blood sugar will thank you.
Do I need to rotate if I use an insulin pump?
Yes, absolutely. Even with a pump, the infusion set is inserted into the same general area for days. Most pump users rotate sets every 2-3 days, but they often reuse the same zone-like always placing it on the lower abdomen. That’s how lipohypertrophy develops in pump users. Rotate your insertion zone weekly, even if you change the set more often.
What’s the best needle size to reduce bruising?
Thinner needles-like 32G or 31G-cause less tissue trauma and reduce bruising. Most modern pens use these sizes. Avoid older, thicker needles (like 28G or 29G) unless your doctor specifically recommends them. Also, make sure your needles are stored properly. Cold or bent needles increase the chance of bruising.
How long does it take to see results after changing injection habits?
You might notice fewer bruises within a week if you stop pressing hard and switch needles. But for lipohypertrophy, it takes 3-6 months of consistent rotation to see visible improvement. Blood sugar stability often improves faster-within 4-8 weeks-as insulin absorption becomes more predictable. Track your A1c, your lows, and your highs. The data will show the difference before your skin does.




Damario Brown
bro i injected in the same spot for 3 years and my belly looks like a deflated basketball. no joke. one day i felt a golf ball under my skin and thought it was a tumor. turned out it was just insulin lumps. doc didn't even check. now i use an app and my lows dropped by like 70%. stop being lazy.
sam abas
interesting article but you completely ignore the fact that most people can't afford to change needles every time. 32G needles cost $0.75 each. that's $22.50 a week. $90 a month. for someone on SSDI? that's rent money. you talk about 'dangerous' lumps like it's a luxury problem. meanwhile, i'm reusing needles because i can't afford to not. your '4-step plan' is a fantasy for people who don't live in real life.
John Pope
let’s be real - this isn’t about insulin. it’s about control. we inject because we’re told to, but our bodies rebel because they sense the violation. every needle is a tiny act of domination over our own flesh. lipohypertrophy? it’s the body’s quiet rebellion. the skin remembers. the fat remembers. the blood remembers. you think you’re managing diabetes? no. you’re negotiating with your own biology. and if you’re not listening… you’re just delaying the reckoning.
the app? the grid? the 1-inch rule? those are just bandaids on a soul wound. the real fix is surrender. stop treating your body like a machine. start treating it like a sacred, scarred temple. then maybe - just maybe - your blood sugar will find peace.
Clay .Haeber
oh wow. another ‘diabetes guru’ with a 4-step plan and a YouTube endorsement. congrats, you’ve turned a medical crisis into a lifestyle brand. ‘Use a fresh needle every time’ - yeah, because I’ve got a trust fund and a subscription to the New York Times. Meanwhile, I’m out here reusing needles like it’s 1998 because my insurance says ‘no’ to 90 needles a month. Also, your ‘grid’? I rotate like a goddamn compass. I just don’t have the luxury of your perfect 2.54 cm precision. This whole thing reads like a TED Talk written by someone who’s never missed a meal.
James Castner
While the clinical insights presented in this article are both empirically sound and clinically significant, I would like to extend the discourse to the broader sociomedical context. The systemic failure to educate patients on injection-site monitoring is not merely an oversight-it is a structural deficit in healthcare delivery. Medical curricula, shaped by cost-driven reimbursement models and time-constrained clinical encounters, have deprioritized patient education in favor of pharmacological intervention. This phenomenon is not unique to diabetes care but reflects a larger epistemological shift in medicine: from holistic stewardship to transactional management. The solution, therefore, must transcend individual behavioral modification and demand institutional reform: mandatory injection-site assessment protocols, insurance coverage for needle replacement programs, and standardized training for primary care providers. Until then, we are merely treating symptoms while the disease of neglect persists.
Adam Rivera
hey man, i’ve been on insulin for 18 years and this stuff saved me. i used to get bruises every week. started using the InPen app, marked every spot, gave each area 6 weeks off. now i barely bruise. also, i just tell my doc: ‘check my belly.’ they’re usually surprised but happy to. you don’t need to be perfect-just consistent. one inch away. fresh needle. no rubbing. it’s simple. not easy, but simple.
lucy cooke
Isn’t it poetic how the very thing meant to sustain us-this life-giving hormone-also becomes the instrument of our body’s slow betrayal? We inject it into our flesh like a prayer, hoping for balance, only to find our skin turning into a map of our neglect. Lipohypertrophy isn’t a medical condition-it’s a monument to the quiet desperation of managing a chronic illness alone. And yet, we keep going. We rotate. We track. We feel for lumps in the dark. We are warriors with syringes and apps. And still, no one asks us how we’re holding up.
Trevor Whipple
you’re all acting like this is rocket science. stop injecting in the same spot. use new needles. don’t press hard. done. if you can’t do that, you’re not sick-you’re just dumb. also, stop complaining about cost. get a job. or stop being a baby. my grandma did this in the 80s with animal insulin and no apps. she didn’t have a ‘grid’-she had grit.
Scottie Baker
you guys are missing the point. it’s not about lumps or bruising. it’s about the fact that we’re treated like broken machines. they give us insulin like it’s a magic bullet and never ask if we’re tired of sticking ourselves 4 times a day. i’ve got scars on my thighs that look like a bad tattoo. i’ve cried in the bathroom after injecting because it hurt too much and i didn’t want to do it again. but i did. because i have to. so don’t lecture me about rotation. just ask me if i’m okay.