Statin Safety Calculator for NAFLD
This tool helps you understand whether your liver enzyme levels are safe for statin therapy based on current medical guidelines. Enter your ALT and AST values (in U/L) to see if you can safely continue or start statins.
According to current guidelines, statins can be safely used even with mildly elevated liver enzymes. The key threshold is 3 times the upper limit of normal (ULN) for ALT and AST. Most people have normal levels between 10-40 U/L, but this can vary by lab.
The FDA removed mandatory liver enzyme monitoring for statins in 2012. Only check liver enzymes at baseline and again at 12 weeks. If levels are below 3x ULN, no further monitoring is needed unless symptoms develop.
Enter your ALT and AST values to see if they're safe for statin therapy.
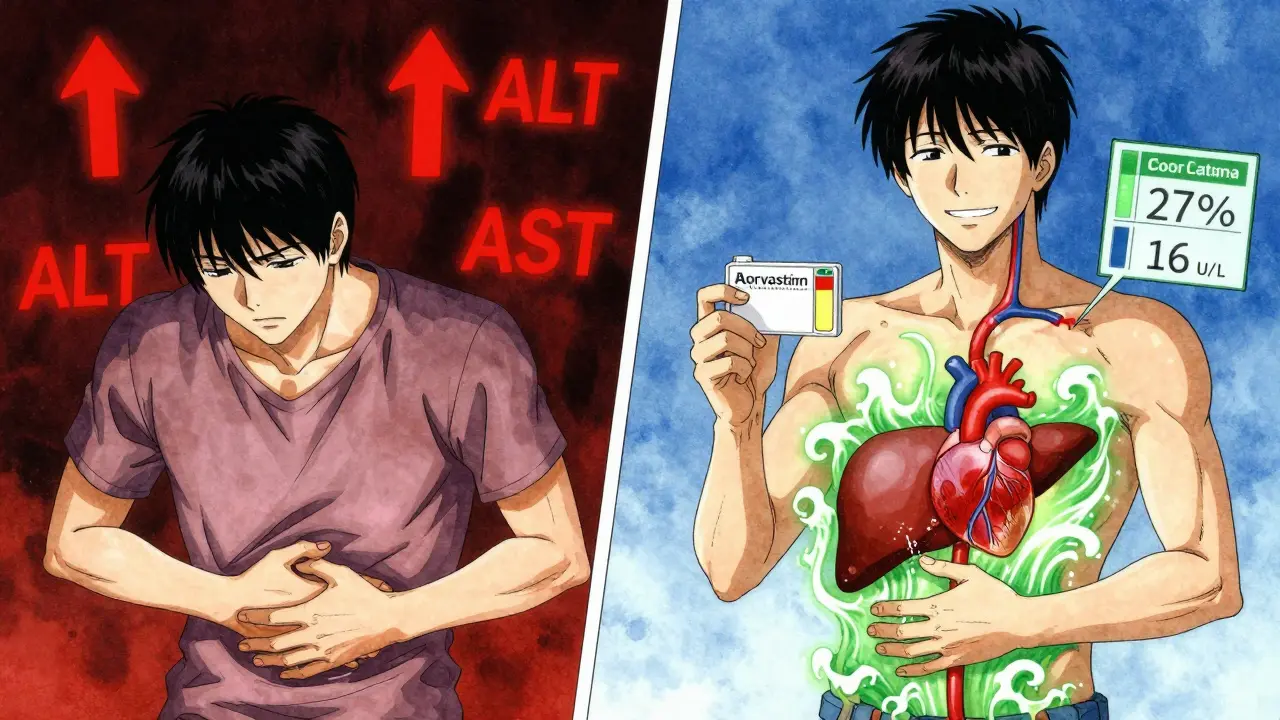
For years, doctors avoided prescribing statins to people with nonalcoholic fatty liver disease (NAFLD). The fear? That these cholesterol-lowering drugs might damage an already stressed liver. But the truth has changed. Today, we know statins are not only safe for most people with NAFLD-they may actually help protect the heart and even slow liver damage. Still, confusion lingers. Many patients are turned away from statins because their liver enzymes are slightly elevated. That’s outdated thinking. Let’s cut through the noise.
Why Statins Are Safe for NAFLD Patients
Statins, like atorvastatin, simvastatin, and rosuvastatin, were never meant to harm the liver. They work by blocking an enzyme in the liver that makes cholesterol. That’s it. Early concerns came from rare cases where statins caused mild, temporary spikes in liver enzymes. But those spikes weren’t signs of damage-they were just signals the body was adjusting. A 2023 analysis of over 200 million research papers found no increased risk of serious liver injury in NAFLD patients taking statins. In fact, the American Association for the Study of Liver Diseases (AASLD), the European Association for the Study of the Liver (EASL), and the European Association for the Study of Diabetes (EASD) all now agree: statins are safe in NAFLD, even if you have mild to moderate fatty liver.How Statins Might Help Your Liver
It’s not just about lowering cholesterol. Statins do more than that. They reduce inflammation and oxidative stress in the liver. Studies show that after six to twelve months on statins, people with NAFLD often see their ALT and AST levels drop-by about 16 U/L and 9 U/L on average. These are the liver enzymes that doctors watch. Lower numbers mean less stress on liver cells. Statins also improve insulin sensitivity, reduce fat buildup in the liver, and may slow the progression of fibrosis. One 2023 review in the National Center for Biotechnology Information found that statins suppress collagen production and lipid peroxide formation-two key drivers of liver scarring. This doesn’t mean statins cure NASH (the more severe form of NAFLD), but they do reduce the risk of it getting worse.Who Should Take Statins? The Real Criteria
You don’t need a perfect liver to qualify for statins. You need high cholesterol, diabetes, high blood pressure, or a history of heart disease. If you have NAFLD and one of those conditions, you’re a candidate. The 2023 AASLD guidelines say: statins are recommended for NAFLD patients with cardiovascular risk factors. That’s it. Liver enzymes alone shouldn’t stop you. The American College of Cardiology and the American Heart Association made this clear back in 2018: elevated liver enzymes are not a reason to avoid statins. In fact, NAFLD patients have a higher risk of heart attack and stroke than people with healthy livers. Skipping statins because of fatty liver is like avoiding seatbelts because you’re worried about a scratch on the car door.Monitoring Liver Enzymes: What You Really Need to Do
Forget monthly blood tests. The old routine of checking liver enzymes every few months isn’t needed. The FDA removed mandatory liver enzyme monitoring for statins in 2012-and most guidelines followed. Here’s what you actually need:- Get a baseline ALT and AST test before starting statins.
- Repeat the test at 12 weeks. If levels are below 3 times the upper limit of normal (ULN), no further monitoring is needed unless you develop symptoms.
- After that, annual checks are enough-unless your doctor suspects another issue.
Why? Because most enzyme changes are harmless. A rise in ALT from 40 to 60 U/L doesn’t mean your liver is failing. It’s noise. Only if levels jump above 3× ULN should you pause and investigate. Even then, it’s often unrelated to the statin. A 2021 Johns Hopkins study of 84 NAFLD patients on statins found that 92% had stable or improved liver enzymes after two years. Only three people stopped the drug because of side effects-and none because of liver problems.
What About Advanced Liver Disease?
If you have cirrhosis, things get a little more nuanced. For compensated cirrhosis (Child-Pugh Class A or B), standard statin doses are still safe. But if you have decompensated cirrhosis (Child-Pugh Class C)-meaning you have fluid buildup, bleeding, or confusion-then lower doses are advised. For example, simvastatin at 20 mg per day instead of 40 mg. Why? Because your liver can’t process drugs as well, and the risk of muscle damage (rhabdomyolysis) goes up by 2.3 times at full doses. That’s not about liver damage-it’s about muscle safety. Your doctor can adjust the statin type and dose based on your liver function. Never assume you’re off-limits. Many people with cirrhosis still benefit from statins if dosed correctly.Statins vs. Other Options
Some doctors reach for fibrates or ezetimibe when they’re nervous about statins. But those drugs don’t have the same heart protection. The GREACE study showed NAFLD patients on statins had a 48% lower rate of heart attacks and strokes compared to those not on statins. That’s huge. Pioglitazone and vitamin E can improve liver histology in NASH, but they don’t reduce heart disease risk like statins do. Statins are the only class of drugs proven to cut mortality in NAFLD patients. A 2023 meta-analysis found a 27% lower risk of death from any cause in those taking statins. That’s not a small benefit-it’s life-changing.Why Do Doctors Still Hesitate?
Despite the evidence, many doctors still avoid statins in NAFLD. A 2023 survey found that 39% of hepatologists require normal liver enzymes before prescribing statins. That’s outdated. Why? Because medical training hasn’t caught up. Most hepatologists didn’t learn this in residency. Meanwhile, cardiologists-who see the heart risks daily-are far more comfortable prescribing them. Only 29% of cardiologists express concern, compared to 68% of hepatologists. Patients often hear, “Your liver enzymes are high, so we can’t give you statins.” That’s not science. That’s habit. The American Liver Foundation’s patient forum has hundreds of stories from people denied statins despite having heart disease. You have the right to ask: “What’s the evidence against this?”
Real-World Results: What Patients Experience
In real life, statins are well-tolerated. In a 2022 Cleveland Clinic study of NAFLD patients on statins, only 8.7% reported muscle aches-similar to the placebo group. Only 1.2% had dangerously high creatine kinase levels, which is the real red flag for muscle damage. Most muscle pain is unrelated to statins. It’s aging, inactivity, or vitamin D deficiency. If you feel muscle soreness, don’t quit statins right away. Talk to your doctor. Check your vitamin D, thyroid, and creatine kinase levels. Often, the fix is simple: switch statins, lower the dose, or take it every other day. Don’t assume it’s the statin. Most of the time, it’s not.What to Do Next
If you have NAFLD and cardiovascular risk factors:- Ask your doctor if you’re a candidate for statin therapy.
- Request your latest liver enzyme results (ALT, AST).
- If they’re below 3× ULN, insist on starting a statin if your heart risk warrants it.
- If they’re higher, ask for a liver ultrasound or FibroScan to check for fibrosis-not just enzyme levels.
- Don’t accept “your liver is too fatty” as a reason to avoid statins.
If you’re already on a statin and have NAFLD: keep taking it. Don’t stop because of a routine blood test. Most changes are harmless. If you’re not on one and have heart disease, diabetes, or high cholesterol, ask why not. The data is clear. Statins save lives in NAFLD. The risk of not taking them is far greater than the risk of taking them.
Looking Ahead
The future is bright. The STANFORD-NAFLD trial, currently recruiting, is testing whether atorvastatin can actually improve liver biopsy results in NASH patients. Early data suggests it can. By 2024, the European Association for the Study of the Liver is expected to formally recommend statins as first-line therapy for heart protection in NAFLD. The treatment gap is huge-only 45% of eligible NAFLD patients get statins, compared to 68% of the general population. That’s over $4 billion in missed prevention every year. We’re not just talking about cholesterol. We’re talking about preventing heart attacks, strokes, and early death in millions of people. Statins aren’t perfect. But for NAFLD patients, they’re one of the most effective tools we have.Are statins safe if I have fatty liver disease?
Yes, statins are safe for most people with nonalcoholic fatty liver disease (NAFLD). Major liver and heart associations now agree they don’t cause liver damage and may even help reduce liver inflammation and fibrosis. The myth that statins harm the liver has been debunked by large studies involving millions of patients.
Should I stop statins if my liver enzymes are high?
No, not unless ALT or AST levels are more than three times the upper limit of normal. Most mild elevations are harmless and unrelated to statins. Guidelines say you can start or continue statins even with moderately elevated enzymes. Only check liver enzymes at baseline and again at 12 weeks-then annually unless there’s a reason to check more often.
Can statins help reverse fatty liver?
Statins don’t directly reverse fatty liver like weight loss or pioglitazone can. But they reduce inflammation, lower fat buildup, and slow fibrosis progression. Studies show they lower liver enzymes (ALT, AST) by 15-20% on average. This means less stress on the liver over time, which can prevent it from worsening into NASH or cirrhosis.
What’s the best statin for someone with NAFLD?
There’s no single “best” statin. Atorvastatin and rosuvastatin are often preferred because they’re potent and not heavily processed by the liver. Simvastatin and lovastatin are metabolized more by the liver, so lower doses are used in advanced liver disease. Your doctor will pick based on your cholesterol levels, kidney function, and liver condition-not just your fatty liver diagnosis.
I have cirrhosis. Can I still take statins?
If you have compensated cirrhosis (Child-Pugh A or B), yes-standard doses are safe. If you have decompensated cirrhosis (Child-Pugh C), use lower doses, like simvastatin 20 mg daily, because your body clears drugs slower. The risk isn’t liver damage-it’s muscle injury. Always work with your doctor to adjust the dose. Many people with cirrhosis benefit from statins for heart protection.
Why do some doctors refuse to prescribe statins for NAFLD?
Many doctors learned outdated information in medical school. A 2023 survey found 39% of hepatologists still require normal liver enzymes before prescribing statins-even though guidelines say otherwise. It’s a knowledge gap, not a safety issue. Cardiologists, who see the heart risks daily, are much more likely to prescribe them. Don’t be afraid to ask for the evidence behind the decision.
Do statins cause muscle pain in NAFLD patients?
Muscle pain happens in about 8-10% of people on statins, but it’s just as common in people not taking them. In NAFLD patients, only 1.2% have dangerous muscle enzyme spikes. Most muscle aches are from aging, low vitamin D, or lack of movement. If you feel pain, don’t quit statins right away. Talk to your doctor. Check your creatine kinase and vitamin D levels. Often, switching statins or lowering the dose helps.
Will taking statins lower my risk of dying from heart disease if I have NAFLD?
Yes. A 2023 meta-analysis found that NAFLD patients on statins had a 27% lower risk of dying from any cause compared to those not taking them. That’s because NAFLD doubles your risk of heart attack and stroke. Statins are the only class of drugs proven to reduce that risk. Not taking a statin when you need one is riskier than taking it.




Juan Reibelo
Finally, someone said it right. I’ve been told my liver enzymes are ‘too high’ for statins-despite having a heart attack in my 40s and diabetes. My cardiologist laughed when I brought up my hepatologist’s concerns. Said, ‘Your liver’s fatty, not broken.’ Took the statin. Enzymes dropped. No muscle pain. Just… life improved. Why are we still treating liver numbers like they’re doom scrolls?
Viola Li
Let’s be real-statins are just another Big Pharma scam. The liver enzyme spikes? Totally normal. But they’re framing it as ‘safe’ to sell more pills. I’ve seen patients crash after taking them. It’s not about evidence-it’s about profit. And now they’re pushing this as ‘standard care’? Please. I’d rather take turmeric and hope.
venkatesh karumanchi
As someone from India where NAFLD is skyrocketing, I’m so glad this info is out there. My uncle had fatty liver and heart disease-he was denied statins for years. Started them last year. His triglycerides are down, his liver enzymes are normal now. He walks 5k steps daily. No drama. Just science. To all doctors: stop overthinking. The data’s here. Help people.
Jenna Allison
Important clarification: the 2023 AASLD guidelines don’t say statins ‘help the liver’-they say they’re safe *in* NAFLD. Big difference. Statins reduce cardiovascular mortality, which is the #1 killer in NAFLD. They don’t reverse steatosis. Pioglitazone or weight loss does that. Don’t conflate heart protection with liver healing. Also-yes, check CK if muscle pain happens. And yes, vitamin D deficiency mimics statin myopathy. Don’t skip the basics.
Kat Peterson
OMG I CRIED. 😭😭😭 After 3 years of being told ‘your liver’s too fatty’-I finally got my statin. My cardiologist said, ‘If your liver could talk, it’d beg you to take this.’ I’m not even mad anymore. Just… grateful. I’m going to the gym tomorrow. And I’m telling my mom to get tested. This changed my life. Thank you for writing this. 🙏❤️
Shelby Marcel
wait so like… if my alt is 80 but im diabetic and have high bp… i can still take statins?? no cap?? i thought i was doomed to heart attack bc my liver was greasy??
blackbelt security
Statins aren’t magic. But they’re the closest thing we’ve got. I’ve seen patients with fatty liver and no other risk factors-fine, hold off. But if you’ve got diabetes, hypertension, or a family history of heart disease? You’re not ‘at risk.’ You’re already in the danger zone. Statins are your seatbelt. Don’t skip it because you’re scared of a scratch.
Patrick Gornik
Let’s deconstruct the epistemology of medical fear. The liver enzyme is a biomarker-not a moral verdict. To refuse statins on its basis is to confuse correlation with causation, and to institutionalize ignorance as precaution. We’ve been conditioned to fear the unknown-yet the data, the meta-analyses, the millions of patient-years-tell a different story. The real pathology isn’t fatty liver. It’s the refusal to evolve. The hepatologist who clings to 1998 protocols isn’t protecting the liver-they’re preserving a dogma. And dogma kills faster than cholesterol.
Luke Davidson
My dad had cirrhosis and was told he couldn’t take statins. He was 68, had a stent, and his LDL was 180. We pushed back. Got him on 10mg rosuvastatin. Two years later, his liver function is stable, his heart’s quiet, and he’s playing with his grandkids again. No muscle pain. No crashes. Just… better. To anyone scared: talk to your doctor. Ask for the guidelines. Don’t let fear make the call. Your heart’s worth more than a number on a lab sheet.
Shanta Blank
Oh please. Let’s not pretend this isn’t a $$$ play. Statins are cheap, patent-free, and profitable for labs that test cholesterol. Meanwhile, the real fix-diet, sleep, stress reduction-isn’t monetizable. So we turn a metabolic disorder into a pill problem. And now we’re gaslighting patients into thinking their liver is fine because enzymes are ‘normal.’ What about the fatty infiltrate? The insulin resistance? The gut dysbiosis? No one talks about that. Statins mask the problem. They don’t fix it. And that’s dangerous.
Kevin Waters
Shoutout to the doc who finally prescribed me a statin after 5 years of ‘maybe next year.’ I had NAFLD, type 2 diabetes, and a 48% 10-year heart risk. They didn’t wait for my ALT to be perfect. They looked at the big picture. I’ve been on it 8 months. My A1c dropped. My triglycerides are half what they were. And I sleep better. No muscle pain. Just… relief. To everyone out there: if you’re eligible, ask. Don’t wait. Your heart doesn’t care about your liver’s opinion.