When you’re expecting, every medication you take feels like a high‑stakes decision. Olmesartan is a popular blood‑pressure pill, but most pregnant women wonder: Olmesartan pregnancy safety - is it a deal‑breaker or can it be managed?
Key Takeaways
- Olmesartan belongs to the angiotensin II receptor blockers (ARBs) class, which the FDA classifies as unsafe in pregnancy.
- Evidence links early‑trimester exposure to increased risk of fetal kidney problems and low birth weight.
- Safer options like labetalol, methyldopa, or hydralazine are recommended for pregnant patients with hypertension.
- If you discover you’ve taken Olmesartan while pregnant, stop the drug immediately and contact your obstetrician.
- Continuous blood‑pressure monitoring and a personalized care plan are essential throughout pregnancy.
What is Olmesartan?
Olmesartan is a prescription medication that belongs to the angiotensin II receptor blocker (ARB) family. It works by blocking the hormone angiotensin II from tightening blood vessels, which helps lower blood pressure.
How Does It Work?
Angiotensin II normally binds to receptors on the smooth muscle of arteries, causing them to constrict. By blocking those receptors, Olmesartan relaxes the vessels, allowing blood to flow more easily. This mechanism is great for adults with high blood pressure but becomes risky when a placenta is involved.
Pregnancy Safety Profile
The crucial question is whether Olmesartan can cross the placenta and affect a developing fetus. Studies show that ARBs, including Olmesartan, do cross the placental barrier and can impair fetal kidney development. The FDA has placed all ARBs in Category D - evidence of risk, but benefits may outweigh risks only in life‑threatening situations.
Key findings from the 2023 WHO pharmacovigilance report:
- Increased incidence of oligohydramnios (low amniotic fluid) when exposure occurs in the first trimester.
- Higher rates of neonatal renal dysfunction and, in rare cases, stillbirth.
- Birth weight averages 200-300 g lower compared to normotensive pregnancies.
Official Guidelines & FDA Stance
Both the American College of Obstetricians and Gynecologists (ACOG) and the FDA advise a complete discontinuation of ARBs as soon as pregnancy is confirmed. The FDA’s FDA label for Olmesartan explicitly states: “If pregnancy occurs, discontinue Olmesartan and consider an alternative antihypertensive.”
Safer Alternatives for Hypertension in Pregnancy
Below is a quick comparison of Olmesartan with three antihypertensive agents that are widely accepted as safe during pregnancy.
| Medication | FDA Pregnancy Category | Mechanism | Typical Dose (Pregnant Women) | Known Fetal Risk |
|---|---|---|---|---|
| Olmesartan | D | Angiotensin II receptor blockade | 20 mg once daily | Renal dysplasia, oligohydramnios, low birth weight |
| Labetalol | Category C (but widely used) | Beta‑blocker + alpha‑blocker | 100‑200 mg 2-3 times daily | Generally safe; monitor for fetal growth restriction |
| Methyldopa | Category B | Central α‑2 agonist | 250‑500 mg 2-3 times daily | Low risk; watch for maternal liver enzymes |
| Hydralazine | Category C | Direct arterial vasodilator | 5‑10 mg 3-4 times daily | Rarely associated with fetal tachycardia |
What to Do If You’ve Taken Olmesartan While Pregnant
- Stop the medication immediately. Do not wait for a refill or another dose.
- Contact your obstetrician or midwife right away. Explain the gestational age and the dose you took.
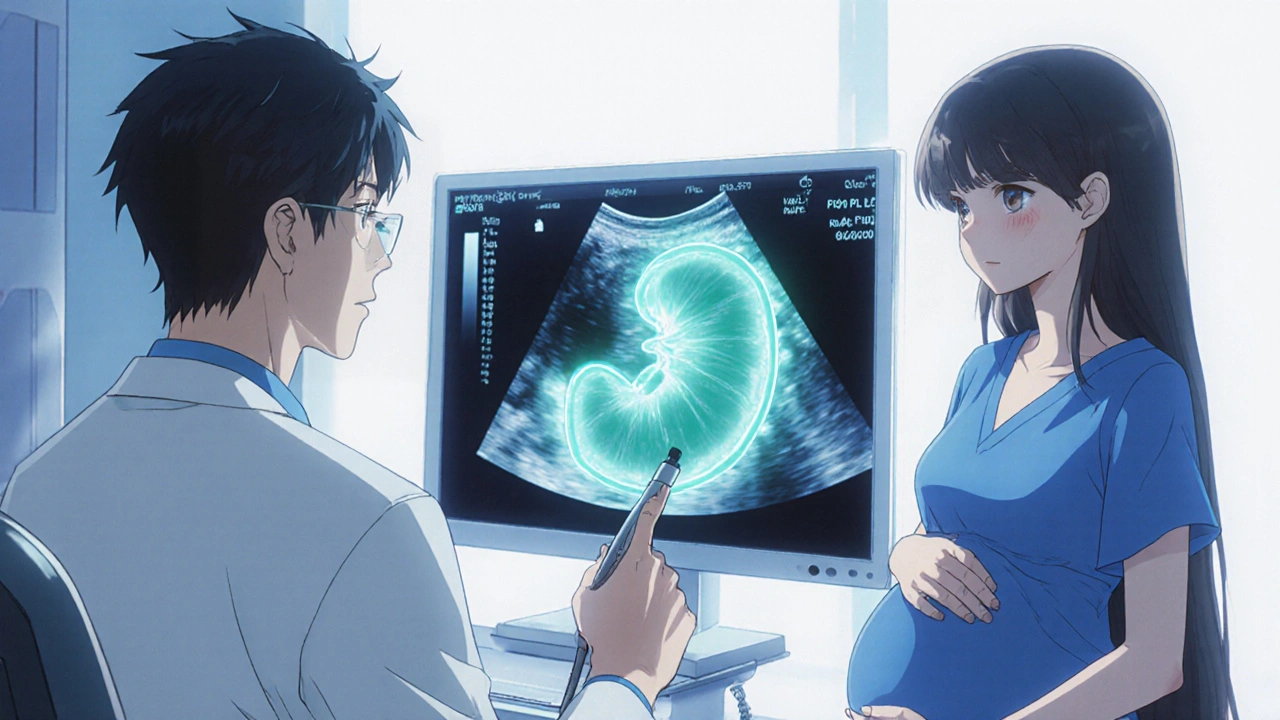
- Expect a thorough fetal ultrasound to assess kidney size, amniotic fluid volume, and overall growth.
- Switch to a pregnancy‑safe antihypertensive under medical supervision.
- Maintain a blood‑pressure log (twice daily) and share it with your care team.
Talking to Your Healthcare Provider
Open communication can make the transition painless. Bring a list of all medications you’re on, including over‑the‑counter supplements. Ask specific questions:
- “What blood‑pressure target should I aim for during each trimester?”
- “How frequently should we do fetal growth scans?”
- “Are there lifestyle tweaks (diet, exercise) that can help reduce my reliance on medication?”
Most doctors appreciate a proactive approach and will gladly adjust your regimen.
Monitoring and Follow‑Up
Pregnancy changes blood volume and heart rate, so blood‑pressure numbers can fluctuate. Here’s a simple monitoring plan:
- First trimester: Check BP at every prenatal visit; home monitoring optional.
- Second trimester: Home BP twice daily (morning & evening). Keep a notebook or app.
- Third trimester: Continue twice‑daily checks; watch for sudden spikes that may signal pre‑eclampsia.
Any reading above 140/90 mmHg should trigger a call to your provider.
Frequently Asked Questions
Is a single dose of Olmesartan harmful?
One accidental dose is unlikely to cause major birth defects, but it still warrants a medical review. The placental transfer begins quickly, so stopping the medication and getting a detailed ultrasound is the safest route.
Can I switch to an ARB after giving birth?
Yes. Once you’re no longer breastfeeding, your doctor can reassess and may re‑introduce an ARB if it’s the best fit for your cardiovascular health.
What are the signs of fetal kidney problems?
Low amniotic fluid (oligohydramnios) on ultrasound, abnormal kidney size, or reduced fetal urine output are red flags. Your doctor will monitor these parameters if exposure occurred.
Are lifestyle changes enough to control blood pressure?
For many pregnant women, diet (low sodium, rich in fruits and vegetables) and gentle exercise (walking, prenatal yoga) can lower BP modestly. However, if your baseline pressure is high, medication is usually still needed.
What does ‘teratogenic’ mean?
Teratogenic describes a substance that can cause birth defects or interfere with normal fetal development.
Bottom line: Olmesartan is powerful for hypertension but carries clear risks during pregnancy. Switching to a safer alternative, staying in close contact with your care team, and monitoring your blood pressure diligently will protect both you and your baby.




Kester Strahan
Olmesartan, as a non‑selective AT1‑receptor antagonist, exhibits high placental permeability due to its lipophilic moiety; the resulting fetal plasma concentrations can approximate maternal levels, thereby perturbing nephrogenesis.
Pharmacokinetic data indicate a volume of distribution (Vd) nearing 1 L/kg, which facilitates trans‑placental transport.
Moreover, the drug's half‑life of ~13 hours sustains steady‑state exposure throughout early organogenesis.
Clinicians should thus prioritize agents with minimal ACE/ARB activity when managing gestational hypertension.
In practice, switching to labetalol or methyldopa mitigates renal dysplasia risk without compromising maternal hemodynamics.
Doreen Collins
Thanks for breaking that down, the pharmacology can feel overwhelming. It really helps to know that there are well‑studied alternatives that keep both mom and baby safe. Staying on top of blood‑pressure logs and having a clear plan with your OB can make the transition seamless. Remember, you’re not alone in navigating this, and your care team is there to support every step.
Dawn Bengel
Pregnant women should never gamble with ARBs 🙅♀️🚫.
junior garcia
Every heartbeat, every tiny kick, deserves the safest care; swapping Olmesartan for a gentle beta‑blocker feels like swapping a thunderstorm for a calm sunrise. Trust the process, trust your doctor, and let the baby thrive.
Dason Avery
Life throws curveballs, but each challenge is a chance to rewrite your health story 🌟. Swapping out a risky med like Olmesartan isn’t a loss; it’s an act of love toward your future child. Embrace the evidence, lean into the safer alternatives, and watch confidence grow with every monitored reading. Your journey becomes a testament that thoughtful choices shape brighter tomorrows.
Casey Morris
Indeed, the literature-though extensive-clearly points to teratogenic potential; consequently, discontinuation is advised, especially once pregnancy is confirmed; moreover, alternative regimens provide comparable efficacy, thereby alleviating concerns, whilst maintaining maternal cardiovascular stability.
Teya Arisa
Dear community, I wish to emphasize the paramount importance of adhering to established clinical guidelines when addressing hypertension in pregnancy. The categorization of olmesartan as a Class D agent underscores the necessity of immediate cessation upon detection of gestation. It is advisable to coordinate with a multidisciplinary team, including obstetrics, cardiology, and pharmacy, to formulate an individualized therapeutic plan. Transitioning to agents such as labetalol, methyldopa, or hydralazine-each with a well‑documented safety profile-will mitigate fetal risk while preserving maternal hemodynamic control. Please ensure frequent ultrasonographic assessments to monitor renal development and amniotic fluid volume. Your vigilance and proactive communication with healthcare providers are essential for optimal outcomes 😊.
HILDA GONZALEZ SARAVIA
Olmesartan, as part of the angiotensin II receptor blocker class, exerts its antihypertensive effect by selectively antagonizing the AT1 receptor on vascular smooth muscle.
This mechanism, while effective in non‑pregnant adults, raises significant concerns during gestation because the renin‑angiotensin system is essential for fetal renal development.
Placental studies have demonstrated that olmesartan traverses the syncytiotrophoblast barrier with a transfer coefficient comparable to that of smaller lipophilic drugs.
Consequently, fetal plasma concentrations can reach up to 70 % of maternal levels within hours of dosing.
Such exposure has been correlated with oligohydramnios, a condition where reduced amniotic fluid reflects impaired fetal urine output.
Oligohydramnios, in turn, predisposes the fetus to pulmonary hypoplasia and musculoskeletal contractures.
Large cohort analyses from the WHO pharmacovigilance database indicate a 2‑fold increase in neonatal renal dysfunction among infants whose mothers took ARBs during the first trimester.
Furthermore, birth weight reductions averaging 250 g have been consistently reported, suggesting a subtle but clinically relevant impact on intrauterine growth.
The FDA’s Category D classification reflects these findings, emphasizing that the drug should only be used when no safer alternative exists.
Clinical guidelines from both ACOG and the European Society of Cardiology recommend immediate discontinuation of olmesartan upon pregnancy confirmation.
Instead, clinicians should consider agents such as labetalol, which offers combined α‑ and β‑adrenergic blockade with a well‑established safety record.
Methyldopa remains another viable option, particularly for patients who experience side‑effects with labetalol.
Hydralazine can be employed in cases requiring rapid afterload reduction, though careful monitoring for maternal tachycardia is warranted.
In practice, a stepwise transition protocol-starting with dose tapering, followed by substitution with a pregnancy‑compatible drug, and concluding with close blood‑pressure surveillance-optimizes maternal cardiovascular stability while protecting fetal development.
Regular ultrasonographic evaluation of fetal kidneys and amniotic fluid volume should be scheduled within two weeks of the medication switch.
Patient education is equally vital; women should be instructed to maintain a home blood‑pressure log and to report any systolic readings above 140 mmHg promptly.
By integrating these strategies, healthcare teams can minimize the teratogenic risk associated with olmesartan and ensure a healthier outcome for both mother and child.