By the end of 2024, more than 277 drugs were still in short supply across the United States. That’s not a glitch. It’s a system failure. Hospitals are rationing antibiotics. Cancer centers are delaying chemotherapy. Emergency rooms are scrambling to find substitutes for basic anesthetics. And behind every shortage is a chain of decisions-some made in Congress, some in federal agencies, some in corporate boardrooms-that have left the country dangerously exposed.
What’s Really Causing the Shortages?
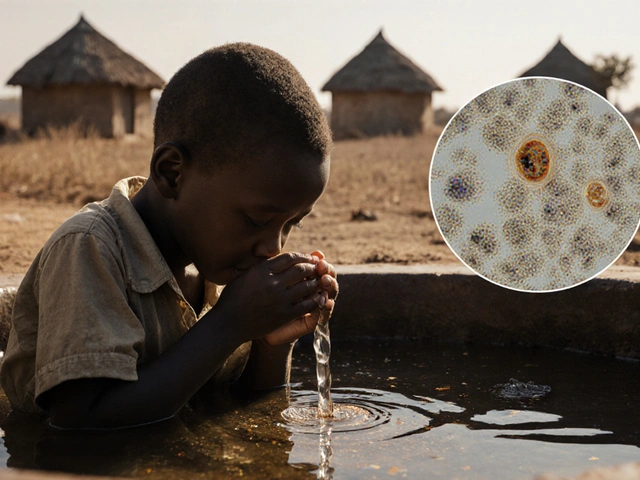
It’s easy to blame bad luck or global supply chain issues. But the real problem is structural. Nearly 80% of the active pharmaceutical ingredients (APIs) used in U.S. medications come from just two countries: China and India. These ingredients are the raw building blocks of drugs-like the flour in bread. Without them, no pill, injection, or IV bag can be made. Even worse, production is concentrated. Just five facilities in the U.S. make 78% of all sterile injectables-drugs given directly into the bloodstream. One factory breaks down, and suddenly hospitals can’t get life-saving antibiotics or heart medications. The FDA says 85% of shortages are resolved through regulatory fixes-like fast-tracking imports or giving manufacturers extra time to fix problems. But those are band-aids. They don’t fix the broken foundation.The Strategic Active Pharmaceutical Ingredients Reserve (SAPIR)
In August 2025, President Trump signed Executive Order 14178, expanding the Strategic Active Pharmaceutical Ingredients Reserve-known as SAPIR. This program doesn’t stockpile finished drugs. It stockspile the raw ingredients needed to make them. Why? Because APIs last 3 to 5 years longer than pills or injections, and they cost 40-60% less to store. SAPIR targets 26 essential medicines: antibiotics like vancomycin, anesthetics like propofol, and oncology drugs like cisplatin. The goal is to have enough raw material on hand to keep production going for at least six months if a foreign supplier cuts off access. The theory makes sense. But here’s the catch: only 12% of critical API production has been brought back to the U.S. since federal efforts began in 2020. And SAPIR’s 26-drug list covers less than 5% of the total drugs that have gone short in the past five years. The FDA’s own data shows that oncology drugs-which made up 31% of all shortages in 2024-are barely represented in SAPIR. Meanwhile, hundreds of other essential drugs, like insulin and dialysis solutions, aren’t even on the radar.How the FDA Is Trying to Fix the System
The FDA runs the Drug Shortage Database, a public tool that tracks every reported shortage. As of November 2025, it lists 1,247 drugs that have had shortages since 2012. Manufacturers are legally required to report potential shortages six months in advance. But only 58% actually do. Small manufacturers-those with fewer than 50 employees-are the worst offenders. Eighty-two percent don’t report at all. Why? Because reporting triggers inspections, delays, and scrutiny. Many can’t afford the paperwork. The FDA has issued only 17 warning letters for non-reporting since 2020. In the European Union, under similar rules, they issued 142. To improve early detection, the FDA launched its Enhanced Shortage Monitoring System in November 2025. It uses artificial intelligence to track shipping data, hospital purchasing trends, and manufacturing batch records. So far, it predicts shortages with 82% accuracy-up to 90 days ahead. That’s a breakthrough. But unless hospitals and pharmacies actually use the alerts, it won’t matter.
Why Congress Is Stuck
Two major bills are sitting in Congress right now: H.R.5316, the Drug Shortage Act, and the bipartisan Drug Shortage Prevention and Mitigation Act. The first would let pharmacists use compounded versions of shortage drugs without waiting for full FDA approval. The second would give Medicare bonus payments to hospitals that keep backup suppliers ready. The Congressional Budget Office estimates H.R.5316 would reduce shortages by 15-20% over five years-at a cost of $740 million. That sounds like a bargain. But total U.S. drug spending is over $1.3 trillion a year. This is less than 0.1% of that. Meanwhile, funding for key agencies is shrinking. The Biomedical Advanced Research and Development Authority (BARDA), which helped develop new manufacturing tech, got a 22% budget cut in the 2026 HHS proposal. FEMA’s emergency response funds were slashed by $1.2 billion. State public health grants dropped by $850 million. You can’t build resilience if you’re pulling the plug on the tools that make it possible.The Real Cost: Hospitals, Pharmacists, and Patients
Hospitals are spending an average of $1.2 million a year just managing drug shortages. That’s not for new equipment or staff-it’s for overtime, emergency purchases, and clinical workarounds. Sixty-eight percent of hospitals report treatment delays. Forty-two percent say patients have gotten the wrong drug because of substitutions. Pharmacists are drowning. The American Society of Health-System Pharmacists found that 74% spend 10 or more hours a week tracking down drugs. One pharmacist on Reddit said they used five different brands of the same antibiotic in a single week. Another had to compound cisplatin from scratch because the FDA-approved version was gone. Patients are paying the price too. Nearly 30% of Americans have skipped doses because a drug wasn’t available-not because they couldn’t afford it, but because it simply didn’t exist on the shelf. Among cancer patients, two out of three have had their treatment changed or delayed due to shortages, according to the National Comprehensive Cancer Network.
What’s Missing: Economic Incentives
Here’s the truth no one wants to say out loud: no company will invest millions to make a drug that earns $0.50 a dose. Sterile injectables-the most common type of shortage-have razor-thin margins. Companies make more money selling a new $10,000 cancer drug than they do selling 100,000 doses of saline solution. The FDA approved 56 new manufacturing facilities in 2024. But 42% of them were overseas-in Ireland, Singapore, and other countries with faster approvals and lower costs. In the U.S., it takes 28-36 months to get a new API plant approved. In the EU, it’s 18-24 months. The only way to fix this is to pay companies to make the drugs we need, not just the ones that make the most profit. That means government contracts, guaranteed minimum purchases, or tax credits tied to producing low-margin essentials. So far, no federal policy has done that.Where Do We Go From Here?
The SAPIR reserve is a good start. The AI-powered monitoring system is smart. But without real investment in domestic manufacturing, without mandatory reporting, without financial incentives for low-profit drugs-we’re just rearranging deck chairs on the Titanic. The EU reduced shortages by 37% between 2022 and 2024 by requiring member states to keep mandatory stockpiles and creating a centralized tracking system. The U.S. could do the same. But it would require political will-and a willingness to spend money before the crisis hits. Right now, the system is built to react, not prevent. And every time a hospital runs out of antibiotics, another patient risks infection. Another cancer patient waits. Another life is put on hold. The tools to fix this exist. The data is clear. The cost of doing nothing? Higher than anyone admits.What is the Strategic Active Pharmaceutical Ingredients Reserve (SAPIR)?
SAPIR is a federal stockpile of raw pharmaceutical ingredients (APIs), not finished drugs. Launched in 2020 and expanded in August 2025, it targets 26 essential medicines like antibiotics, anesthetics, and cancer drugs. The goal is to keep production going during supply chain disruptions by storing cheaper, longer-lasting ingredients instead of finished products.
Why are drug shortages still rising despite federal efforts?
Federal efforts focus on reacting to shortages, not preventing them. Only 12% of critical API production has been brought to the U.S. despite seven years of initiatives. The SAPIR reserve covers just 5% of shortage-prone drugs. Manufacturing is still concentrated in a few facilities, and companies have no financial incentive to produce low-margin drugs. Reporting requirements are weak, and funding for prevention has been cut.
How does the FDA track drug shortages?
The FDA maintains a public Drug Shortage Database that lists all active and resolved shortages. Manufacturers are legally required to report potential shortages six months in advance. In November 2025, the FDA launched an AI-powered monitoring system that analyzes shipping data, hospital orders, and manufacturing records to predict shortages 90 days ahead with 82% accuracy.
Why don’t more companies report potential shortages?
Reporting triggers FDA inspections and regulatory scrutiny, which can delay production. Small manufacturers-with fewer than 50 employees-are especially reluctant, with 82% failing to report. The FDA has issued only 17 warning letters for non-reporting since 2020, compared to 142 in the EU under similar rules. There’s little consequence for ignoring the law.
What’s the biggest barrier to fixing drug shortages?
The biggest barrier is economics. Companies make little to no profit on essential, low-cost drugs like antibiotics and saline solutions. There’s no financial reward for investing in redundant manufacturing, even when lives are at risk. Until the government creates guaranteed markets or subsidies for these drugs, shortages will keep happening, no matter how many stockpiles or AI tools are created.







Wendy Chiridza
The SAPIR reserve is a step in the right direction but it's still way too narrow. They're focusing on 26 drugs when over 277 are in shortage. Why not expand it to include insulin dialysis solutions and common antibiotics that patients actually rely on every day? It's not just about cancer drugs it's about basic care
Pamela Mae Ibabao
Let's be real here the FDA's AI system is cool but it's useless if hospitals don't act on it. I work in a rural ER and we get zero alerts. The system is built for big city hospitals with IT departments not for the places where shortages hurt the most
Gerald Nauschnegg
Look I get the economic argument but you can't just hand out tax credits and expect companies to play nice. The real issue is that the FDA approval process is a nightmare. It takes 3 years to get a new API plant approved here but 2 years in the EU. That's not policy that's bureaucracy with a side of incompetence
And don't even get me started on how Congress keeps cutting funding to BARDA while pretending they care about drug security. It's performative politics at its worst
Palanivelu Sivanathan
Bro this whole system is rigged. The corporations are laughing all the way to the bank while we're scrambling for saline bags. China and India control the APIs because we outsourced everything for cheap profits. Now we're paying with lives. It's not a shortage it's a betrayal. The FDA is just a puppet. The real power is in the boardrooms of Pfizer Merck and the Chinese state-owned pharma giants. We're not in a crisis we're in a colonial extraction economy
And they want to fix it with AI? Please. The answer isn't algorithms it's revolution. We need to nationalize API production. End of story. No more profits over people
Joanne Rencher
Ugh I'm so tired of this. We've known about this for a decade. Why is this even a debate? Just make companies build more factories. Done. Why does everything have to be so complicated
Erik van Hees
Actually you're all missing the point. The real problem is the FDA's outdated regulatory framework. They still treat APIs like they're in the 1980s. Modern manufacturing can be decentralized modular and automated. We could have 100 small regional API plants if the FDA stopped treating every new facility like a nuclear reactor. The EU does it. Why can't we? It's not about money it's about mindset
Cristy Magdalena
I just lost my mom to a delayed chemo cycle because cisplatin was out. They gave us a substitute that didn't work. The FDA says they're working on it. Working on it? My mom is dead. And you're talking about AI predictions and tax credits? This isn't a policy problem. This is a moral failure. And I'm not going to stop screaming until someone listens
Adrianna Alfano
My cousin is a pharmacist in Ohio and she told me she spent 14 hours last week just trying to find one antibiotic. She had to call 12 different distributors. One time she got it from Canada. Another time she had to compound it from powder. And she's not even getting paid extra for this. It's insane. We treat healthcare like a commodity but people aren't products. This system is breaking hearts every day
Casey Lyn Keller
Let me guess the next thing they'll say is that we need more data. We already have the data. We've had it for years. The real reason nothing changes is because the people in charge don't want it to. The same people who profit from the status quo are the ones writing the rules. This isn't incompetence. It's intentional
Jessica Ainscough
Just want to say thank you to everyone working on the front lines. Pharmacists nurses ER docs you're carrying this whole system on your backs. I know it feels like no one sees you but people are seeing you. We're listening. We're not giving up. We need to keep pushing
May .
SAPIR is a bandaid
Sara Larson
WE CAN DO THIS 🙌 Let's push Congress to pass H.R.5316 now! $740 million is NOTHING compared to the cost of lives lost. We need guaranteed purchases for low-margin drugs. We need faster approvals. We need to bring production home. This isn't a dream it's a plan. Let's make it happen 💪❤️
Josh Bilskemper
Let's be honest the entire premise is flawed. The U.S. doesn't need to produce every API. Globalization exists for a reason. Efficiency. If India can make vancomycin cheaper and faster why are we wasting billions on domestic production? The real issue is logistics not manufacturing. We should be investing in strategic stockpiles and rapid transport networks not rebuilding 1950s industrial policy