Every year, millions of people rely on generic drugs to manage everything from high blood pressure to chronic pain. They’re cheaper, widely available, and legally required to work the same as brand-name versions. But behind the low price tag is a hidden risk: contamination. In 2022, nearly 1 in 5 drug recalls in the U.S. were linked to contamination-and over a third of those involved generic medications. This isn’t about rare mistakes. It’s about systemic gaps in a global supply chain that’s stretched thin, underfunded, and hard to monitor.
What Exactly Is Generic Drug Contamination?
Contamination means something unwanted ends up in your pill, capsule, or cream. It could be chemical residues from a previous batch, tiny particles from dirty equipment, bacteria from untrained staff, or even toxic impurities like nitrosamines. The FDA defines it as the unintended introduction of impurities from the environment, other drugs, or the manufacturing process itself. It doesn’t matter if the drug is generic or brand-name-the law says both must be pure. But in practice, generics face more pressure to cut costs, and that’s where risks creep in.Take a simple example: a factory makes metronidazole for infections, then switches to a blood pressure pill without fully cleaning the machines. Leftover chemical traces from the first drug can end up in the second. That’s cross-contamination. Or imagine a worker in a cleanroom sheds 40,000 skin cells per minute. Those cells carry bacteria. If the gowning process is sloppy, those microbes can end up in your antibiotic. The FDA says 75-80% of particles in cleanrooms come from people. That’s not science fiction-it’s daily reality in many facilities.
Why Are Generic Drugs More at Risk?
Generic drug makers operate on razor-thin margins. While brand-name companies can spend 60-70% of revenue on R&D and quality, generics often make only 20-25%. That means less money for clean equipment, better training, or advanced testing. In 2022, FDA inspections found 8.3% of generic manufacturing sites had contamination-related violations-compared to just 5.1% for brand-name facilities. In India, where most active ingredients are made, the rate jumped to 12.7%.Older facilities are a big problem. Plants built before 2000 are 34% more likely to have contamination issues. Many still use open production lines where powders are poured by hand. Newer companies like Teva in Italy reduced cross-contamination by 78% by switching to fully closed systems-where the drug never touches the air. But that costs $500,000 to $2 million per line. Most small generic makers can’t afford it.
There’s also the supply chain. About 80% of the active ingredients in U.S. drugs come from just two countries: India and China. The FDA inspects only 1% of imported drugs. That means most shipments sail through without being tested. In 2018-2019, a single impurity called nitrosamine contaminated 22 generic versions of a blood pressure drug across eight countries. Over 2,300 products were recalled. Total cost: $1.2 billion. And that was just one chemical.
How Contamination Happens: The Real-World Pathways
It’s not just about dirty machines. Contamination happens in quiet, overlooked ways:- Piercing vials: When pharmacists or nurses stick needles into drug vials, they can pull in tiny particles or microbes. This caused 62% of hazardous drug contamination incidents.
- Breaking ampules: Glass shards and microscopic debris can get into the liquid when a sealed glass container is snapped open. This was linked to 28% of incidents.
- Inadequate cleaning: Cleaning validation requires proving you removed at least 10 parts per million of the previous drug. But many facilities skip full testing. One pharmacy in Texas found copper specks in generic metronidazole tablets-later traced to uncleaned mixing tanks.
- Poor air control: Non-sterile drugs should be made in ISO Class 8 environments (like a clean office). Sterile drugs need ISO Class 5-equivalent to a hospital operating room. Many generic plants fall short.
Microbial limits are strict: no more than 1,000 bacteria or 100 mold spores per gram in oral pills. But testing can take 7 days. By then, the batch is already shipped. Top manufacturers now use rapid microbiological methods that give results in 4 hours. But only 63% of leading generic makers have adopted them.
What You Can Do: Prevention Starts With Awareness
You can’t inspect every pill. But you can be smarter about how you use and question your meds:- Check the manufacturer: Look at the pill imprint or packaging. Some generic makers have better reputations. Teva, Mylan, and Sandoz have invested heavily in contamination controls. Smaller, unknown brands? Be cautious.
- Watch for changes: If your pill suddenly looks different-new color, specks, odd smell-don’t take it. Contact your pharmacist. One patient developed severe skin rashes after switching to a contaminated hydrocortisone cream. The FDA confirmed copper and fungal contamination.
- Report anything strange: Use the FDA’s MedWatch system. Between 2020 and 2022, over 1,200 reports were filed about possible contamination in generics. Some led to recalls. Your report could save someone else’s life.
- Ask your pharmacist: Pharmacists are on the front lines. In a 2022 survey, 28% of hospital pharmacists said they’d seen suspicious generics. If your pharmacist seems unsure or hesitant, dig deeper.
How the System Responds When Things Go Wrong
When contamination is found, the FDA can force a recall. But the system is reactive, not proactive. Most recalls happen only after someone gets sick or a lab finds something wrong. The MedWatch system collects patient and provider reports. If enough red flags appear, the FDA investigates.Manufacturers must notify the FDA within 24 hours of discovering contamination. They’re required to recall affected batches under 21 CFR Part 7. But here’s the catch: recalls don’t always reach every pharmacy. In rural areas, stock might still be on shelves for weeks. And not all recalls are publicized clearly. Some just appear as a quiet update on the FDA website.
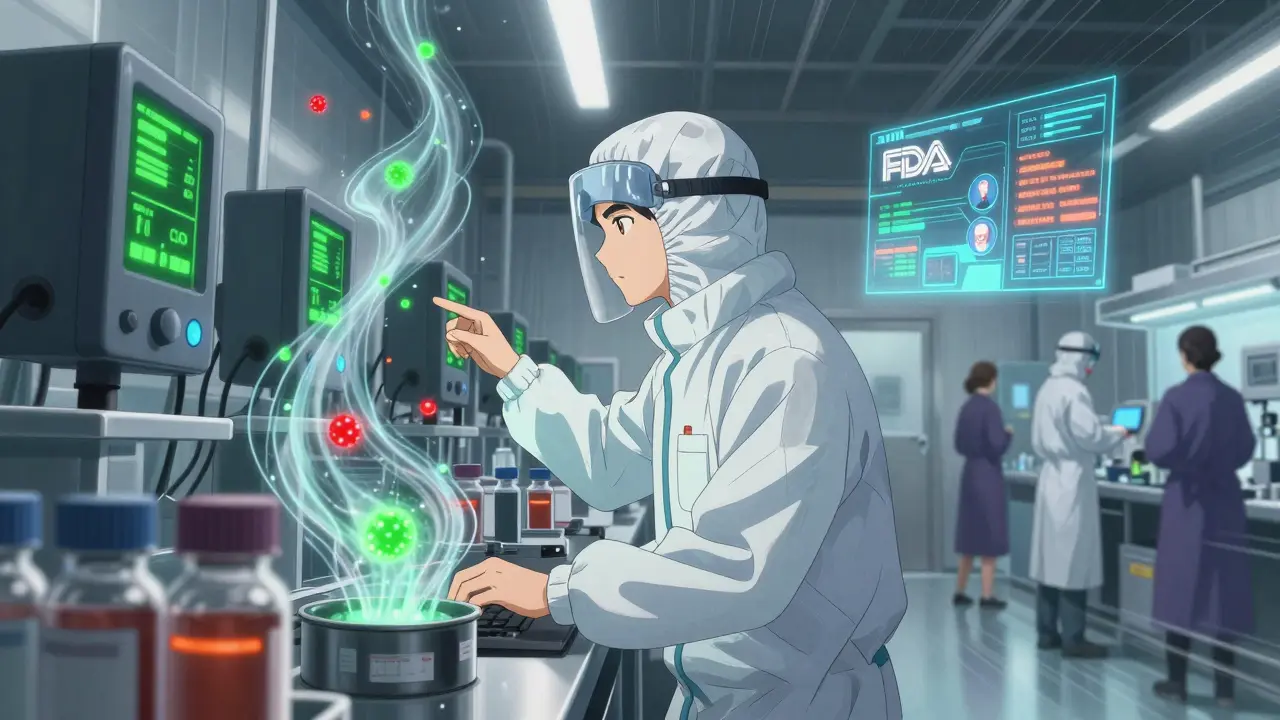
Big manufacturers are now using AI to predict contamination. The FDA’s new Digital Transformation Initiative uses machine learning to analyze 15,000+ data points from environmental sensors-temperature, humidity, particle counts, airflow. By 2024, this system will flag high-risk facilities before contamination happens. It’s already 89% accurate in trials.

What’s Changing for the Better
There’s progress, even if it’s slow:- Strict nitrosamine testing: Since January 2023, all sartan-class blood pressure drugs must be tested for cancer-causing impurities.
- Improved inspection tools: The FDA’s PREDICT system now flags 37% more risky imports than before.
- Stronger cleaning rules: New USP guidelines require disinfectants to kill bacterial spores, not just surface germs.
- Real-time monitoring: Mylan’s Morgantown plant cut contamination by 82% using live particle counters and better gowning protocols.
By 2027, industry analysts predict contamination-related recalls will drop by 40%. But experts warn: supply chain complexity won’t disappear. More drugs will come from more places. More pressure will be on regulators to keep up.
Final Thought: Safety Isn’t Just a Label
Generic drugs saved the U.S. healthcare system over $300 billion in the last decade. They’re essential. But safety isn’t guaranteed just because a pill is cheap. The system relies on manufacturers doing the right thing, regulators having enough resources, and patients speaking up when something feels off.If your medication doesn’t work like it used to-if you feel worse after switching brands-don’t ignore it. Talk to your doctor. Ask your pharmacist where the drug was made. Report it. The next person who takes that pill might be your parent, your child, or you.
Can generic drugs be as safe as brand-name drugs?
Yes, they can-and often are. The FDA requires generics to have the same active ingredient, strength, dosage form, and performance as the brand-name version. The problem isn’t equivalence-it’s contamination. Some generic manufacturers have better quality control than others. The issue isn’t the generic label-it’s the factory, the supply chain, and the investment in safety.
How do I know if my generic drug is contaminated?
You usually can’t tell by looking. But watch for unusual changes: strange colors, spots, odd smells, or pills that dissolve differently. If you feel worse after switching to a generic-new nausea, rash, dizziness, or no effect-you may have a contaminated batch. Don’t assume it’s your body. Report it to your pharmacist and the FDA’s MedWatch system.
Are all generic drugs made in India or China?
No, but most active ingredients are. About 80% of the raw chemicals in U.S. drugs come from India and China. The final pills might be packaged in the U.S., but the key component-the part that makes the drug work-is often made overseas. Some U.S.-based manufacturers make generics too, but they’re fewer in number and often more expensive.
What should I do if I think my medication is contaminated?
Stop taking it. Keep the bottle and any packaging. Contact your pharmacist-they can check if there’s a recall or known issue. Then report it to the FDA through MedWatch (medwatch.fda.gov). Even one report can trigger an investigation. If you’ve had a reaction, see your doctor immediately and mention the possibility of contamination.
Is it worth paying more for brand-name drugs to avoid contamination?
Not necessarily. Many brand-name drugs have had contamination issues too. The difference is often in manufacturing practices, not the brand name. A well-run generic maker can be safer than a poorly managed brand-name one. Focus on the manufacturer, not the label. Ask your pharmacist which generic brand your pharmacy carries and look up their recall history.
How often are generic drug factories inspected?
The FDA inspects U.S. facilities every 2-5 years. For foreign plants-where most ingredients come from-it’s about once every 10 years on average. Less than 1% of imported drug shipments are physically tested. That’s why contamination often goes undetected until someone gets sick.








Katie Schoen
So let me get this straight-we’re trusting our life-saving meds to factories where people shed 40k skin cells a minute and no one’s checking if the machines were cleaned? 🤡 I mean, I’d rather get my blood pressure pills from a guy in a van than some of these places.
Molly McLane
I’ve been a pharmacist for 18 years and I’ve seen this firsthand. One batch of generic metformin had visible specks-turned out it was copper from uncleaned tanks. Patients blamed their diabetes for ‘getting worse.’ No one asked where it came from. We need better labeling. Not just the brand-name the factory. Period.
Rachel Wermager
The FDA’s current microbial limits (100 mold spores/g) are based on outdated ISO 11137 standards from 1998. Modern rapid microbiological methods (RMMs) like ATP bioluminescence or qPCR can reduce turnaround from 7 days to 4 hours, yet adoption remains below 63% due to capital expenditure constraints and regulatory inertia. The real bottleneck isn’t contamination-it’s the failure to implement validated process analytical technology (PAT) frameworks across the global supply chain.
Harshit Kansal
In India, we make 40% of the world’s generics. Factories here? Some are clean, some are chaos. But you think Americans don’t have issues? Last year, a U.S. plant recalled 2 million pills because the cleaning crew used dish soap instead of pharmaceutical-grade detergent. It’s not about where it’s made-it’s about who’s watching.
Brian Anaz
This is why we need to ban all imports from China and India. We’re letting foreign labs poison our kids just to save $20 on a prescription. American workers can make these drugs safely. Stop outsourcing safety for profit. Build the plants here. Pay the workers. End this.
Saylor Frye
I mean, if you’re going to take a generic, you’re basically playing Russian roulette with your liver. I read the FDA’s 2022 inspection reports. The photos of the cleanrooms? Looked like a high school science lab after prom. I’d rather pay double and know my pills weren’t made next to a dumpster.
Katie Schoen
I just got my new generic lisinopril and the pill looks like it was rolled in glitter. I called my pharmacy-they said ‘different batch.’ I said ‘but the last one didn’t taste like metal.’ They hung up. So now I’m just taking it and hoping I don’t start hallucinating.
Tom Swinton
I just want to say-thank you to every pharmacist who speaks up, every patient who reports a weird pill, every nurse who double-checks the label. You’re the only thing standing between people and poison. I’ve seen patients get sick because they didn’t know to ask where their meds came from. Please, if you’re reading this-ask. Always ask. And if you’re scared? Write it down. Send it to MedWatch. It matters more than you think.
Joann Absi
THEY’RE POISONING US!!! 🚨💀 This isn’t healthcare-it’s a corporate horror movie! India and China are running drug factories like they’re making cheap sneakers! I’m not taking another pill until the U.S. bombs every foreign plant and brings back manufacturing to AMERICA!!! 🇺🇸🔥 #DrugWar #NoMorePoisonPills
Venkataramanan Viswanathan
As someone who grew up in a village where medicine was a luxury, I am deeply grateful for generics. But I also know that quality cannot be sacrificed for cost. In India, many small manufacturers lack resources, but the government is now enforcing GMP with blockchain traceability. Change is slow, but it is coming. We must support ethical producers, not punish entire nations.