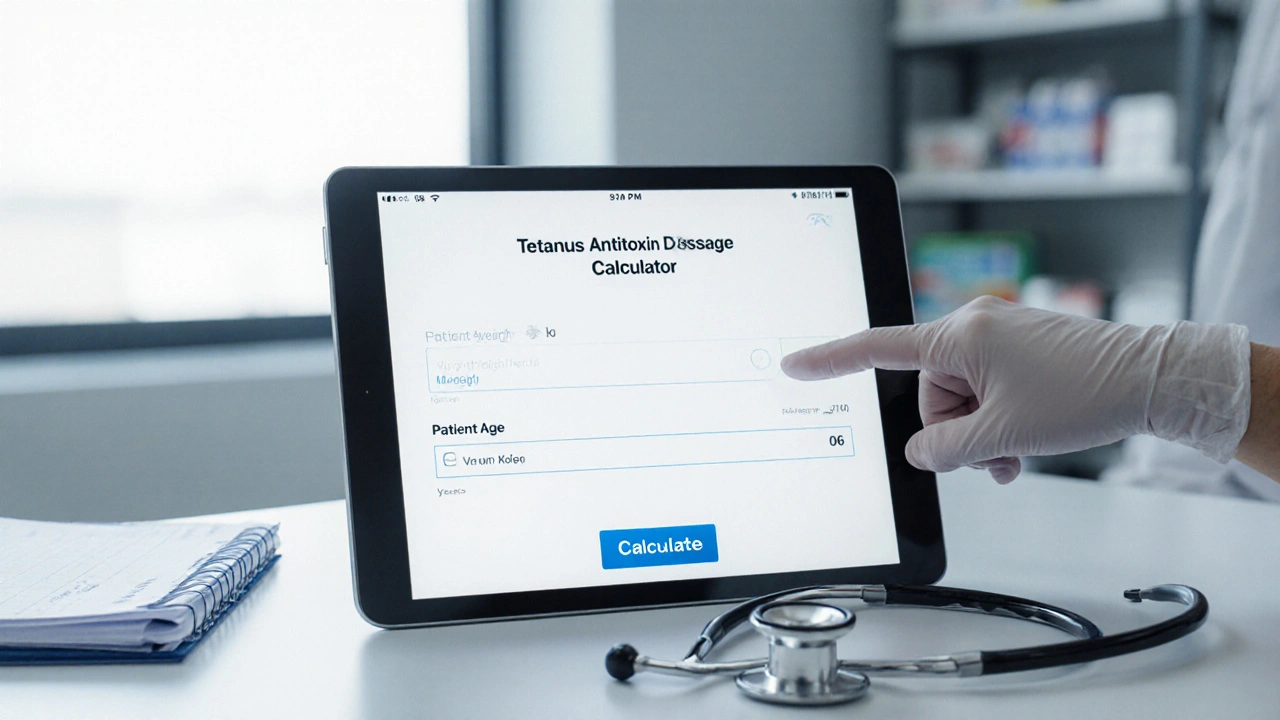
Tetanus Antitoxin Dosage Calculator
Patient Information
Recommended Dose
The calculated dose of tetanus antitoxin is:
This should be administered intramuscularly, preferably in the deltoid muscle for adults or anterolateral thigh for children.
Quick Takeaways
- Tetanus antitoxin provides immediate, short‑term protection by neutralising circulating tetanus toxin.
- It is indicated for high‑risk wounds, cases where vaccination status is unknown, or when a patient cannot mount an active immune response.
- Dosage is weight‑based and must be given intramuscularly, preferably in the deltoid muscle.
- Common side effects are mild (pain, redness); severe reactions are rare but require prompt medical attention.
- Guidelines from the WHO and CDC keep the antitoxin central to early tetanus management while emphasising vaccination for long‑term immunity.
When a wound is contaminated with Clostridium tetani, the bacterium that causes tetanus, the toxin it releases can trigger severe muscle spasms and, if untreated, can be fatal. The body’s own antibodies take several days to develop after vaccination, leaving a dangerous gap. That’s where Tetanus Antitoxin a preparation of ready‑made antibodies that instantly neutralise circulating tetanus toxin steps in. It works as a form of passive immunisation, buying time for the patient’s immune system or a vaccine to kick in.
How Tetanus Antitoxin Works
The antitoxin is derived from the plasma of horses or, more recently, from human donors. Each unit contains high‑titer immunoglobulins that bind to the tetanus toxin’s active site, preventing it from attaching to nerve endings. This neutralisation stops the cascade that leads to the classic lock‑jaw and generalized muscle rigidity.
Because the antibodies are pre‑formed, the effect is immediate-usually within minutes. However, the protection lasts only as long as the antibodies remain in circulation, typically 2-4 weeks. For lasting immunity, a tetanus toxoid vaccine is required to stimulate the patient’s own B‑cells to produce antibodies.
When to Use Tetanus Antitoxin
Guidelines converge on a few key scenarios:
- Deep, contaminated, or puncture wounds where the patient’s vaccination history is incomplete or unknown.
- Severe burns, necrotic tissue, or crush injuries that provide an anaerobic environment for bacterial growth.
- Patients with compromised immune systems who cannot rely on an active vaccine response.
- Clinical suspicion of tetanus infection before laboratory confirmation.
In practice, clinicians assess the wound, ask about the last tetanus booster (usually recommended every 10years), and then decide whether to give antitoxin alone, antitoxin plus vaccine, or just the vaccine.
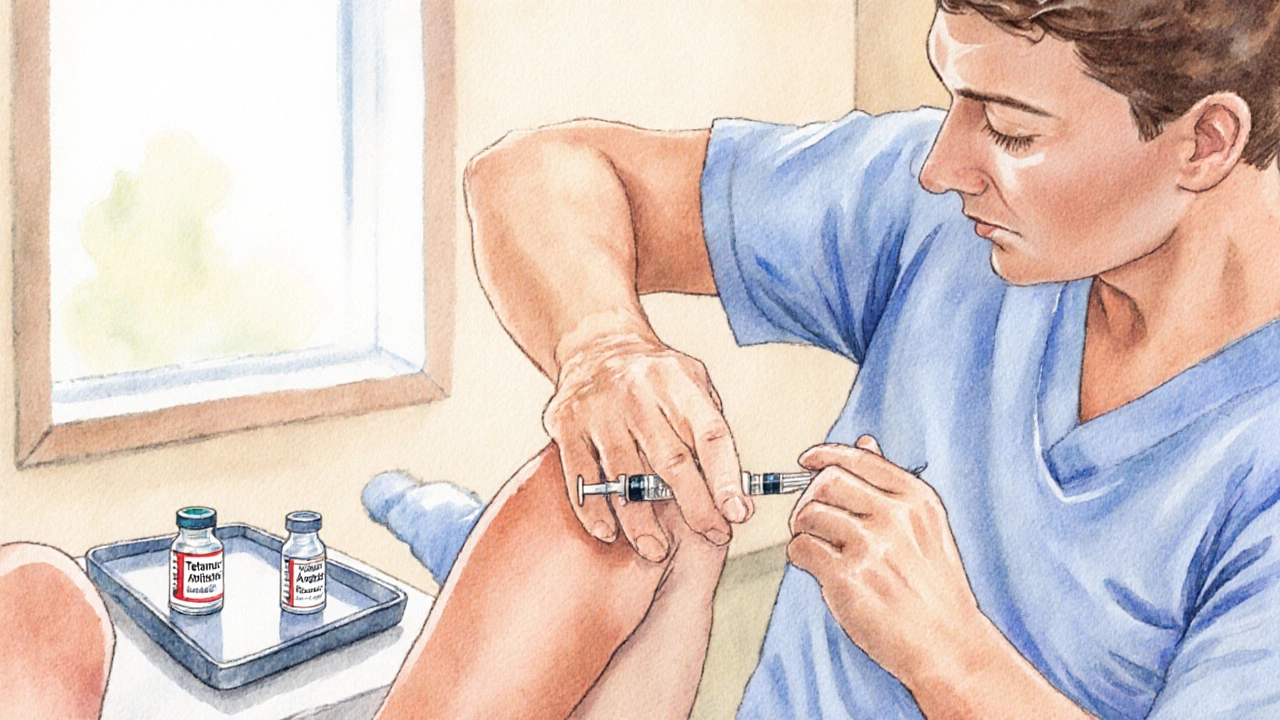
Dosage and Administration
Standard dosing follows body‑weight calculations. For adults, 3000IU of antitoxin is typical; children receive 500-1000IU depending on age and weight. The product is reconstituted with sterile water and injected intramuscularly, preferably into the deltoid muscle to ensure rapid absorption.
- Confirm the patient’s weight and calculate the appropriate IU dose.
- Reconstitute the antitoxin vial according to the manufacturer’s instructions.
- Choose a clean injection site (deltoid for adults, anterolateral thigh for infants).
- Administer the dose slowly; monitor the patient for any immediate reactions.
- Document the administration, including batch number and expiry date.
After giving the antitoxin, the patient should receive a tetanus toxoid booster within the next 7‑10days to establish active immunity.
Safety Profile and Side Effects
Because the antitoxin originates from animal or human plasma, allergic reactions can occur. Most patients experience mild local discomfort, redness, or a low‑grade fever that resolves within 24hours.
Severe reactions-such as anaphylaxis, serum sickness, or bronchospasm-are rare (<0.1% of administrations) but must be treated promptly with epinephrine, antihistamines, and supportive care. Pre‑screening for known hypersensitivity to horse serum can reduce risk.
Contraindications include:
- Documented severe allergy to equine proteins.
- Previous anaphylactic reaction to tetanus antitoxin.
In such cases, clinicians may opt for human‑derived tetanus immune globulin (TIG) instead.
Comparison with Other Immunisation Strategies
Below is a side‑by‑side look at the three main tools used to prevent or treat tetanus.
| Feature | Tetanus Antitoxin | Tetanus Immune Globulin (TIG) | Tetanus Toxoid Vaccine |
|---|---|---|---|
| Source | Equine plasma (most common) or human plasma | Human plasma‑derived | Inactivated tetanus toxin (toxoid) |
| Onset of protection | Minutes (neutralises existing toxin) | Minutes | 4-7 days for antibody production |
| Duration of effect | 2-4 weeks | 2-4 weeks | Years (boosters every 10) |
| Typical dose (adult) | 3000IU | 250IU | 0.5mL (0.5LFC) |
| Risk of severe allergy | Low‑to‑moderate (horse protein) | Very low | Negligible |
| Cost (USD) | ~$15‑$25 per vial | ~$30‑$45 per vial | ~$5‑$10 per dose |
In emergency situations, the antitoxin or TIG is chosen for rapid neutralisation. For long‑term protection, the vaccine remains the gold standard.
Guidelines from Global Health Authorities
The World Health Organization (WHO) recommends a single dose of 3000IU tetanus antitoxin for all high‑risk wounds when vaccination history is uncertain. The Centers for Disease Control and Prevention (CDC) aligns closely but adds a note that in countries with reliable immunisation records, a booster alone may suffice for clean minor wounds.
Both bodies stress the importance of:
- Wound debridement and proper cleaning.
- Early administration of antitoxin within 24hours of injury.
- Completion of a tetanus toxoid series (3 doses) for lasting immunity.
In Australia, the National Immunisation Program follows the same principles, with the antitoxin reserved for cases where the patient’s last booster was >10years ago or documentation is missing.
Common Misconceptions
1 “If I get the tetanus vaccine, I never need antitoxin.” The vaccine protects against future infection but does not neutralise toxin already in the bloodstream. In a fresh wound, antitoxin may still be required.
2 “Antitoxin can replace the vaccine.” The antitoxin provides only temporary protection; without vaccination, the patient remains vulnerable to later exposures.
3 “All tetanus treatments are the same.” Each product-antitoxin, TIG, vaccine-has a distinct role, dosage schedule, and safety profile.
Practical Tips for Clinicians
- Keep a stocked fridge with both antitoxin and TIG to handle allergic patients.
- Use a pre‑filled syringe for the antitoxin to reduce preparation errors.
- Document every dose, including lot number, to assist with pharmacovigilance.
- Educate patients on the need for a follow‑up vaccine dose within a week.
- Review local infection control policies; some regions have specific antitoxin dosing algorithms.
Frequently Asked Questions
What is the difference between tetanus antitoxin and tetanus immune globulin?
Tetanus antitoxin is usually derived from horse plasma, while tetanus immune globulin (TIG) comes from screened human donors. Both neutralise toxin, but TIG carries a much lower risk of severe allergic reactions.
How quickly does antitoxin work after injection?
Neutralisation begins within minutes because the antibodies are already formed, providing immediate protection against circulating toxin.
Can I give the antitoxin to a child who is under 5 years old?
Yes, but the dose is weight‑based-typically 500-1000IU for children. Always follow local pediatric dosing guidelines and monitor for reactions.
Do I still need the tetanus vaccine after receiving antitoxin?
Absolutely. Antitoxin offers short‑term protection only. A tetanus toxoid booster should be given within 7‑10 days to create lasting immunity.
What are the signs of a severe allergic reaction to antitoxin?
Look for hives, swelling of the face or throat, difficulty breathing, or a sudden drop in blood pressure. Treat immediately with epinephrine and call emergency services.
Understanding the role of tetanus antitoxin helps clinicians make fast, evidence‑based decisions when a patient presents with a potentially contaminated wound. Combine rapid toxin neutralisation with proper wound care and the tetanus toxoid series, and the odds of severe disease drop dramatically.

Jesse Goodman
Toxin fights no one, but the antitoxin helps us keep our nerves calm. 😅
Antara Kumar
While the calculator looks fancy, relying on it blindly ignores the nuances of local treatment protocols, especially in Indian rural clinics where resources differ.
John Barton
Oh great, another web‑app promising to solve tetanus with a few clicks – because we all know physicians love spreadsheets more than real judgment.
Achint Patel
In the grand tapestry of medicine, a dosage is but a number, yet the decision to inject hinges on the story behind the wound.
Remember, the deltoid isn’t just a muscle; it’s the launchpad for recovery when the immune system is on standby.
Every patient carries a unique microbiome that subtly influences toxin susceptibility.
The weight‑based 300 IU/kg rule is a blunt instrument, not a scalpel.
When you factor in age, nutritional status, and comorbidities, the picture becomes far more intricate.
Clinicians should ask themselves whether the calculated dose truly reflects the pathogen load.
Over‑administration can provoke hypersensitivity reactions, while under‑dosing leaves the toxin unchecked.
Guidelines exist for a reason, but they are built on population averages, not individual narratives.
In low‑resource settings, the cost of antitoxin may dictate a more conservative approach.
Conversely, in high‑risk trauma cases, a higher initial dose can buy critical time.
The route of administration-deltoid for adults, anterolateral thigh for children-optimizes absorption, but improper technique nullifies the benefit.
Healthcare teams must train on proper intramuscular injection depth to avoid sub‑optimal delivery.
Follow‑up serology, though rarely done, can confirm whether protective antitoxin levels were achieved.
Ultimately, the calculator is a tool, not a replacement for clinical judgment.
Use it wisely, and always cross‑check with the patient’s overall clinical picture.
Lilly Merrill
Interesting tool – I’ve seen similar calculators used in community clinics here, and they do help streamline the dosing process when the staff is stretched thin.
Charlie Martin
Just a heads‑up: the 300 IU/kg rule may overshoot for lightweight teenagers; double‑checking with pediatric guidelines is wise.
Danielle Watson
The interface looks clean but the script could use a comment for the weight conversion it’s confusing some users
Kimberly :)
Actually, the missing comment isn’t a bug; it’s a deliberate minimalism to keep the page lightweight 😊.
Sebastian Miles
From a pharmacokinetic view, tetanus antitoxin has a half‑life of ~7‑10 days, so a single calculated dose covers the acute phase.
Harshal Sanghavi
Sure, but remember that in practice you still need to consider wound grading; a high‑risk puncture may call for booster alongside the calculated antitoxin.