When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how do regulators know it’s truly the same? The answer lies in two numbers: Cmax and AUC. These aren’t just jargon-they’re the backbone of every generic drug approval worldwide. If these two values don’t match within strict limits, the drug won’t get approved. And that’s not just bureaucracy-it’s about your safety.
What Cmax Tells You About a Drug’s Peak
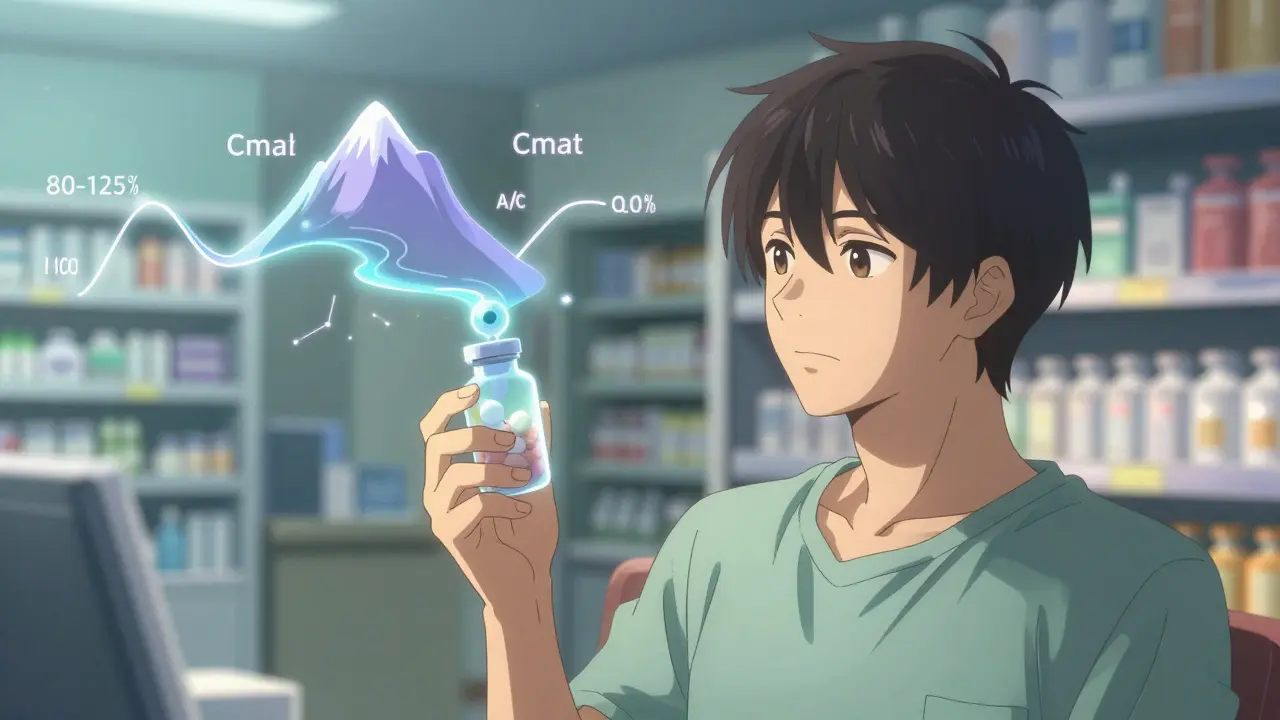
Cmax stands for maximum concentration. It’s the highest level of a drug in your bloodstream after you take it. Think of it like the peak of a mountain you climb. If you’re taking a painkiller, this peak determines how fast you feel relief. If you’re on a drug with a narrow safety window-like warfarin or digoxin-this peak can mean the difference between healing and harm.
For example, if a brand-name drug hits a Cmax of 8.1 mg/L, the generic must come very close. Regulators don’t just want it to be similar-they demand it fall within 80% to 125% of the original. So if the brand hits 8.1, the generic must land between 6.5 and 10.1. Anything outside that range? It gets rejected. Why? Because too low might mean no effect. Too high? You risk toxicity.
But here’s the catch: Cmax doesn’t just depend on the drug itself. It’s shaped by how fast the pill breaks down, how well it dissolves, and even what you ate before taking it. That’s why bioequivalence studies control diet, timing, and even whether you’re fasting. A single late blood draw during the absorption phase can throw off the whole result. Studies show that 15% of failed bioequivalence tests happen because sampling didn’t catch the true peak.
What AUC Reveals About Total Drug Exposure
AUC-area under the curve-is the total amount of drug your body is exposed to over time. Imagine tracing the entire path of the drug’s journey in your blood, from the moment it enters to when it’s almost gone. The space under that curve? That’s AUC. It’s measured in mg·h/L, meaning how much drug is in your system, multiplied by how long it stays there.
AUC matters most for drugs that work cumulatively. Antibiotics, antivirals, and many chronic disease meds rely on sustained exposure. If your AUC is too low, the drug doesn’t stay long enough to do its job. Too high? You might build up toxic levels over days or weeks. Unlike Cmax, which is a single snapshot, AUC is a full story. That’s why regulators require it alongside Cmax. One tells you how fast you get there. The other tells you how much you get overall.
Take a common example: a generic version of a cholesterol-lowering drug. The innovator shows an AUC of 124.9 mg·h/L. The generic? 112.4 mg·h/L. That’s a 90% ratio-well within the 80-125% range. So it passes. But if it were 75%, regulators would say no. Even if the drug seems to work in a small trial, the data says: don’t risk it. The science is clear: small differences in exposure add up, especially over years of daily use.

Why Both Metrics Are Non-Negotiable
You might think: if AUC is total exposure, why do we even care about Cmax? Because drugs don’t all behave the same. Some need a quick spike to activate receptors-like fast-acting insulin or painkillers. Others need steady, low levels over time-like antidepressants or blood pressure meds. AUC alone can’t tell you if the drug hits too fast or too slow. Cmax fills that gap.
Regulators don’t let one pass if the other fails. Both must meet the 80-125% rule independently. There’s no averaging. No compromise. If a generic has the right AUC but its Cmax is 130%? Rejected. If Cmax is perfect but AUC is 78%? Also rejected. This isn’t arbitrary. It’s based on decades of clinical data showing that even small deviations in either parameter can lead to real-world problems-like seizures from too-high peak levels or treatment failure from too-low exposure.
The standard 80-125% range didn’t come from guesswork. It was shaped by statistical models and real-world outcomes. In 1991, experts from around the world met and agreed: a 20% difference in exposure isn’t clinically meaningful for most drugs. That’s why the limits are symmetrical on a log scale-ln(0.8) = -0.2231, ln(1.25) = 0.2231. It’s math that matches biology.
What Happens When the Rules Don’t Fit
Not all drugs fit neatly into this system. Some, like warfarin or levothyroxine, have such a narrow safety margin that even a 10% change can cause bleeding or thyroid crashes. That’s why the EMA now allows tighter limits-90-111%-for these high-risk drugs. The FDA is considering the same.
Then there are drugs with high variability. Some people absorb them quickly. Others barely absorb anything. For these, the standard 80-125% rule can unfairly block good generics. That’s why regulators now allow something called scaled average bioequivalence. It stretches the limits based on how variable the drug is. But it’s not automatic. It needs strong data. And even then, it’s only for a handful of drugs.
One 2021 study looked at 500 bioequivalence trials. It found that 82% of generics matched the brand within 90-110% for AUC. But Cmax? Only 78% did. That small drop tells you something important: the rate of absorption is harder to control than total exposure. That’s why labs sample blood every 15-30 minutes in the first few hours-because missing the peak by even 15 minutes can change everything.

How Studies Are Done-And Why Timing Matters
Every bioequivalence study follows the same script. Around 24 to 36 healthy volunteers take both the brand and generic versions in a random order, with a washout period in between. Blood is drawn 12 to 18 times over 24 to 72 hours. The key? Sampling during the absorption phase. If you don’t take samples at 0.5, 1, 1.5, and 2 hours, you might miss the true Cmax. And if you do, the whole study fails.
Modern labs use LC-MS/MS machines that can detect drugs at levels as low as 0.1 nanograms per milliliter. That’s like finding one grain of salt in an Olympic swimming pool. This precision is why today’s generics are so reliable. But it also means mistakes are costly. A single poorly timed sample can cost a company millions and delay access to affordable medicine.
Most studies use a two-period crossover design. Each volunteer gets both drugs. This cuts down on individual variation. Statistical analysis then uses log-transformed data because drug concentrations don’t follow a normal bell curve-they follow a log-normal one. You can’t just average them. You have to transform them first. Most labs now use software like Phoenix WinNonlin. It’s not magic-it’s math. But it’s math that’s saved millions of lives.
The Bigger Picture: Why This Matters to You
Over 1,200 generic drugs were approved in the U.S. alone in 2022. Almost all of them passed because of Cmax and AUC. These numbers are why you pay $5 for a pill that costs $50 as a brand. Without this system, generics wouldn’t be trusted. And without generics, millions wouldn’t be able to afford treatment.
But this isn’t just about cost. It’s about consistency. A patient switching from brand to generic-and back again-needs to know their medication won’t suddenly stop working or cause side effects. Cmax and AUC make that possible. They’re the invisible gatekeepers of drug safety.
Even with new tech like modeling and simulation, regulators aren’t ditching these metrics. As Dr. Robert Lionberger of the FDA said in 2022: "AUC and Cmax will remain the primary bioequivalence endpoints for conventional drug products for the foreseeable future." Why? Because they’ve been tested, validated, and proven for over 40 years. No other metric comes close.
The system isn’t perfect. But it’s the best we have. And for now, it’s the reason you can trust that little white pill on your nightstand.
Why do regulators require both Cmax and AUC instead of just one?
Cmax tells you how fast the drug enters your bloodstream-important for drugs where timing affects safety or effectiveness, like painkillers or seizure meds. AUC tells you how much total drug your body absorbs over time-critical for drugs that need steady levels, like antibiotics or antidepressants. Using both ensures the generic matches the brand in both speed and total exposure. If only one were used, you might get a drug that works the same overall but hits too fast (risking side effects) or too slow (reducing effectiveness).
What does the 80-125% range mean in bioequivalence?
It means the generic drug’s Cmax and AUC must be within 80% to 125% of the brand-name drug’s values. For example, if the brand has an AUC of 100 mg·h/L, the generic must be between 80 and 125. This range is based on statistical analysis showing that differences smaller than 20% are unlikely to affect clinical outcomes. The limits are symmetrical on a log scale because drug concentrations follow a log-normal distribution-not a normal one-so logarithmic transformation is required for accurate analysis.
Can a generic drug pass bioequivalence if only one metric (Cmax or AUC) meets the criteria?
No. Both Cmax and AUC must independently meet the 80-125% range. Regulators require both because they measure different things: rate of absorption (Cmax) and total exposure (AUC). If one fails, the drug is considered not bioequivalent-even if the other passes perfectly. This rule prevents situations where a drug might have the right overall exposure but an unsafe peak concentration, or vice versa.
Why is sampling timing so critical in Cmax measurements?
Cmax is a single point in time-the highest concentration in the blood. If blood samples are taken too infrequently or too late, you might miss the true peak. For fast-absorbing drugs, Cmax can occur within an hour. Missing the 1-hour or 1.5-hour sample can lead to underestimating Cmax by 20% or more. Studies show that poor sampling during the first 1-2 hours causes about 15% of bioequivalence study failures. That’s why protocols require frequent sampling-often every 15-30 minutes-early on.
Are there exceptions to the 80-125% rule?
Yes. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or cyclosporine-regulators tighten the range to 90-111%. Small changes in exposure can cause serious side effects or treatment failure. Also, for drugs with high variability (where absorption differs greatly between people), regulators may allow scaled bioequivalence, which adjusts the limits based on how variable the drug is. But these exceptions are rare, require strong evidence, and are only applied to specific drug classes.






Khaya Street
Cmax and AUC? Yeah, I’ve read the FDA guidelines. Honestly, most people don’t realize how much math and blood draws go into making that $5 generic pill. It’s not magic-it’s statistics, precision, and a whole lot of fasting volunteers.
And yeah, missing a single 1.5-hour sample can tank a whole study. I’ve seen labs redo entire trials because of one late draw. It’s wild how fragile the data is.
Still, I’m glad they don’t cut corners. I’d rather pay a little more for something I know won’t kill me.