Autoimmune hepatitis isn’t something you catch from someone else. It’s not caused by alcohol, viruses, or poor diet. It’s your own immune system turning against your liver. Think of it like a security guard who forgets the rules and starts attacking the building they’re supposed to protect. The liver gets inflamed, scarred, and slowly loses function - unless you stop it early. The good news? We know how to do that. The standard treatment - steroids and azathioprine - has been saving lives since the 1970s. But it’s not simple. It’s a balancing act between stopping the immune attack and avoiding serious side effects.
How Do Doctors Know It’s Autoimmune Hepatitis?
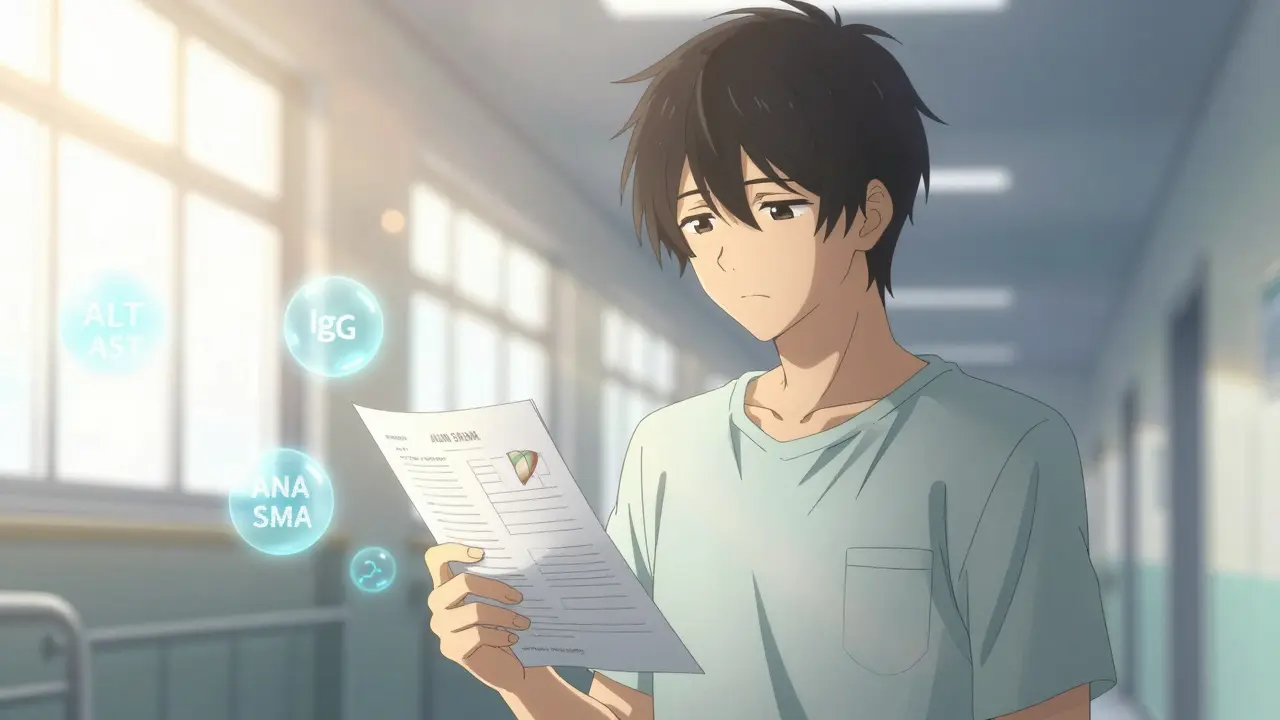
There’s no single blood test that says, “Yes, this is autoimmune hepatitis.” Instead, doctors piece together clues like a detective. First, they check liver enzymes - ALT and AST. In active disease, these are usually 5 to 10 times higher than normal. That tells them the liver is damaged, but not why. Next, they look at immunoglobulin G (IgG). If it’s more than 1.5 times the upper limit of normal, that’s a red flag. Then come the autoantibodies: ANA and SMA are the most common, found in about 80% of cases. LKM1 antibodies show up in the other 20%, usually in younger patients. But here’s the twist: the 2025 European Association for the Study of the Liver guidelines say you don’t need to classify the type based on these antibodies anymore. They don’t change how you treat it.
The real confirmation comes from a liver biopsy. Not just any scan - a needle biopsy, done under ultrasound guidance. The pathologist looks for interface hepatitis: inflammation right where the liver’s portal areas meet the healthy tissue. If you see this in at least 20 portal tracts, it’s textbook. You also rule out everything else: hepatitis B and C, alcohol use, fatty liver, medications. The Revised International Autoimmune Hepatitis Group (IAIHG) scoring system adds it all up - symptoms, blood tests, biopsy, exclusions. A score above 15 means probable AIH. Above 20? Definite. That’s when treatment starts.
Why Steroids Are the First Line of Defense
Prednisone (or prednisolone) is the go-to steroid. It works fast. Most patients feel better within days. Liver enzymes drop noticeably in just two weeks. That’s not just a coincidence - it’s proof the immune system is being suppressed. The typical starting dose is 0.5 to 1 mg per kilogram of body weight per day, up to a max of 60 mg. That sounds high, and it is. But it’s temporary. The goal isn’t to stay on this dose forever. It’s to get the inflammation under control, then reduce it as quickly as possible.
By week 8, doctors aim to taper it down to 10-15 mg daily. Why? Because steroids have a long list of side effects. Weight gain. Moon face. Insomnia. Mood swings. Bone thinning. Diabetes. About 70% of people on steroid-only treatment develop at least one major side effect within five years. That’s why adding azathioprine isn’t optional - it’s essential.
How Azathioprine Makes Steroids Safer
Azathioprine (brand name Imuran, or generic azathioprine) is an immunosuppressant. It doesn’t work fast. It takes weeks to months to build up in your system. But once it does, it lets you cut your steroid dose by 70-80%. That’s huge. Instead of staying on 30 mg of prednisone, you can drop to 5-10 mg. Side effects drop from 70% to 30%. That’s the power of combination therapy.
The usual starting dose is 50 mg per day, slowly increased to 1-2 mg per kg per day - max 150 mg. But before you even start, there’s a critical step: TPMT enzyme testing. About 0.3% of people have a genetic variant that makes them unable to break down azathioprine. If they take it, their bone marrow shuts down. That’s life-threatening. Testing for this costs $250-$400 in the U.S., and while 89% of academic centers do it now, many community clinics still skip it. Don’t let that be you. Ask for the test.
Side effects of azathioprine are different: nausea, fatigue, pancreatitis, low white blood cells. One patient on Reddit described it as “pancreatitis at 100 mg - had to switch.” That’s why dose increases are slow and blood counts are checked every 2-4 weeks early on.
How Long Do You Stay on Treatment?
This is where things get messy. Most people think, “If my blood tests look good, I’m cured.” Not true. Biochemical remission - normal ALT, AST, and IgG - usually takes 18 to 24 months. But that doesn’t mean the disease is gone. The inflammation may be quiet, but the immune system hasn’t forgotten. That’s why the 2025 EASL guidelines say: don’t rush to stop treatment. Evaluate response between 6 and 12 months, not just at 6. Some people need longer.
After 2-3 years of stable remission, some doctors try to wean you off. But here’s the hard truth: 50-90% of patients relapse if they stop completely. Only about 45% stay in remission two years after stopping. That’s why 60-80% of people stay on low-dose maintenance therapy for life. It’s not ideal. But it’s safer than cirrhosis or liver failure.
And yes - repeat biopsies are still the gold standard to confirm histological remission. That means no more interface hepatitis. Studies show 50-70% of patients reach this after 2-3 years. One patient on HealthUnlocked said: “After two years on 5mg prednisone + 75mg azathioprine, my biopsy went from F3 fibrosis to F0.” That’s the kind of outcome we’re fighting for.
What If It Doesn’t Work?
Most people respond. But 10-15% don’t. That’s called treatment failure. Or sometimes, they can’t tolerate the side effects. When that happens, second-line drugs kick in. Mycophenolate mofetil (CellCept) is the most common alternative. It’s often better tolerated than azathioprine. Dose: 1-1.5 grams twice daily. Calcineurin inhibitors like tacrolimus are another option. Both have their own side effect profiles - kidney issues, high blood pressure - but they work when the first line fails.
And new drugs are coming. Obeticholic acid (Ocaliva) got FDA breakthrough therapy status in 2024. Early trials show a 42% complete response rate versus 28% with standard therapy. JAK inhibitors like tofacitinib and IL-6 blockers like clazakizumab are in phase 2 trials. They’re not approved yet, but they’re the future.

What You Need to Do Before and During Treatment
Before starting immunosuppressants, you need two vaccines: hepatitis A and B. Why? Because if you get infected while on these drugs, your body can’t fight it. And if you’ve had hepatitis B in the past (even if you’re negative now), you’re at risk for reactivation. That’s why doctors test for HBsAg and anti-HBc before treatment. If positive, you get antivirals like tenofovir to prevent a dangerous flare.
Monitoring is non-negotiable. Blood tests every 2-4 weeks at first. Then every 3 months. IgG every quarter. Bone density scans if you’re on steroids long-term. Eye exams for cataracts. Diabetes screening. And yes - if you’re on azathioprine, your blood counts must be watched like a hawk. Low white cells? Lower the dose. Platelets dropping? Pause it.
And don’t ignore mental health. One patient said: “The insomnia felt like permanent jet lag.” Mood swings, fatigue, body image issues - these are real. They’re part of the disease and the treatment. Talk to your doctor. Get support. You’re not alone.
The Big Picture: Progress and Hope
Autoimmune hepatitis used to be a death sentence. Now, with early diagnosis and proper treatment, most people live normal lifespans. The global market for AIH drugs is growing - $1.2 billion in 2024, projected to hit $1.8 billion by 2029. Why? Because more people are being diagnosed. More are staying on treatment. And more are surviving.
The 2025 EASL guidelines are a game-changer. They simplify diagnosis. They extend the treatment response window. They emphasize patient-centered care. They push for genetic testing. They recognize that quality of life matters as much as liver enzymes.
Yes, steroids make you gain weight. Yes, azathioprine can make you nauseous. But for most, the trade-off is worth it. Your liver is healing. Your future is safer. And science is getting better every year.








Peyton Feuer
man i just found out my cousin got diagnosed with this last year. she was terrified, thought she was gonna die or something. but after 18 months on prednisone + azathioprine, her enzymes are normal and she’s hiking again. the side effects sucked at first - moon face, insomnia, the whole deal - but she says it was worth it. just wish more docs pushed the TPMT test before starting azathioprine. my cousin’s doc skipped it and she got sick as a dog for weeks. lucky she didn’t crash her bone marrow.
Mandy Kowitz
oh wow, so we’re just gonna poison people with steroids and hope they don’t turn into potatoes? genius. next you’ll tell me we should inject them with lead for ‘liver health.’ i mean, sure, it works - but only because we’ve given up on actually curing anything. just slap a bandaid on the immune system and call it a day. classic medicine.
Justin Lowans
This is an exceptionally well-articulated overview of autoimmune hepatitis management. The integration of diagnostic criteria with therapeutic timelines reflects a nuanced understanding of chronic immune-mediated pathology. I particularly appreciate the emphasis on histological remission as a gold standard - biochemical normalization alone is insufficient to declare disease quiescence. The data on relapse rates post-tapering underscores the necessity of long-term, low-dose maintenance in the majority of patients. It is heartening to see guidelines evolve toward patient-centered outcomes rather than purely laboratory-driven endpoints.
Michael Rudge
Wow, so you’re telling me the medical establishment still hasn’t figured out how to make people feel like human beings while treating them? You give someone 60mg of prednisone, turn them into a puffy, sleep-deprived zombie, then hand them azathioprine like it’s a vitamin - and call it ‘standard of care’? And you wonder why people distrust doctors? This isn’t medicine - it’s chemical containment. Someone’s gotta invent a cure, not just a chemical leash.
Angie Rehe
Let’s clarify: the 2025 EASL guidelines explicitly de-emphasize antibody subtyping because it lacks clinical utility - not because it’s irrelevant. The diagnostic algorithm is now streamlined: IgG elevation + interface hepatitis on biopsy + exclusion of other etiologies = AIH. No need for over-testing. And yes, TPMT testing is non-negotiable - if your clinic isn’t doing it, they’re operating outside of evidence-based practice. My lab requires it before any thiopurine initiation. Period. No exceptions. If you’re not getting tested, you’re gambling with your neutrophils.
Enrique González
Just wanted to say - if you’re on this treatment, you’re not broken. You’re fighting. Every blood test, every side effect, every sleepless night - it’s all part of the battle. I’ve been on 5mg prednisone + 75mg azathioprine for 4 years. My biopsy went from F3 to F0. I still have bad days. But I’m alive. I’m here. And I’m not giving up. You got this.
Aaron Mercado
Wait - so you’re telling me you’re gonna give me a drug that can KILL MY BONE MARROW… and you don’t test for it first?!?!?!?!?!?!?!!? That’s not negligence - that’s criminal. I’ve seen people die from this. Not from the disease - from the treatment. And now you want me to trust a system that still skips TPMT testing in 11% of clinics?!?!? This isn’t healthcare - it’s Russian roulette with a syringe.
saurabh singh
From India here - we don’t have access to all these fancy tests or drugs, but we still treat AIH with steroids + azathioprine. It works. My uncle was diagnosed 8 years ago. He’s still going strong on low-dose meds. Yes, he gained weight. Yes, he had nausea. But he’s alive. He plays with his grandkids. That’s the win. We don’t have Ocaliva or JAK inhibitors here… but we have hope. And that’s enough for now. Keep pushing for better - but don’t forget what’s already saving lives.